Collections are a balancing act.
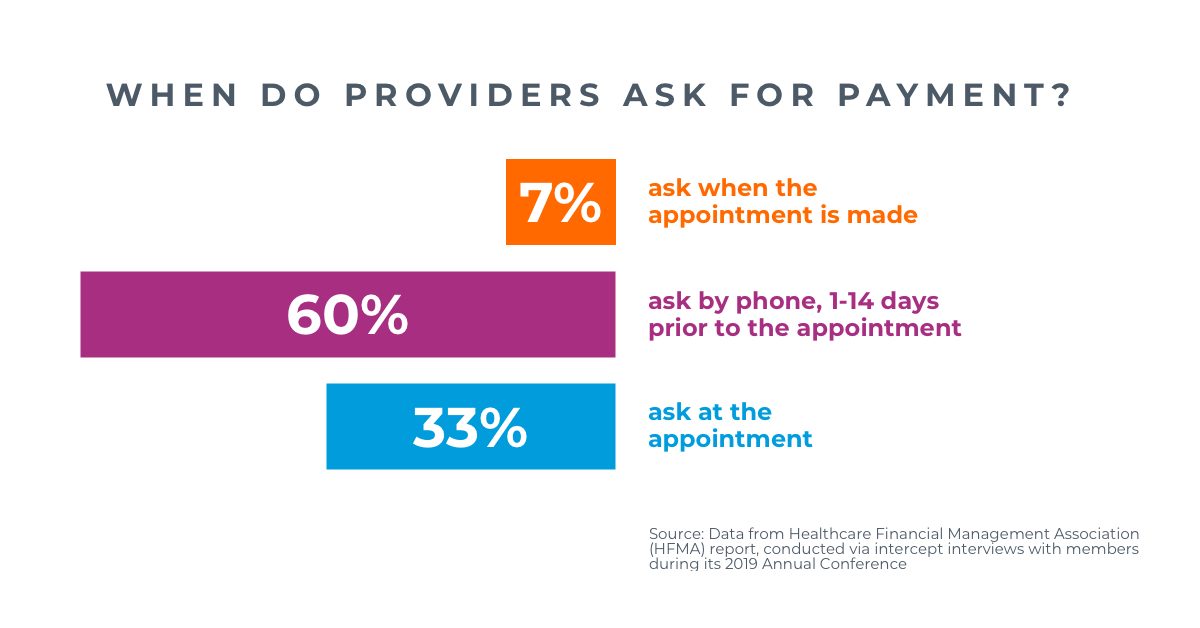
“If your point-of-service (POS) collections start at the point of service, you’re already behind,” says Eric Sulivant, solution strategist at Waystar. “But if you reach out too early, too often, or you’re using a communication method your patients don’t prefer, patient satisfaction declines.”
So how do you strike the right balance?
Learn 4 ways to improve point-of-service collections
POS collections pro-tip:
1. Start with accurate estimates
How confident are you in your estimation data? What’s your accuracy rate? Do your tools get smarter over time?
When it comes to point-of-service collections, accuracy is imperative. If your system doesn’t give you quick, correct information about eligibility, pre-authorizations, and coverage detection, your estimates will suffer — and that can sink your patient satisfaction.
Nearly two in three patients (60%) will consider switching providers if the estimates they get are inaccurate. And, if you’re arming your staff with incorrect information, there’s no amount of compassion they can show to counteract a patient’s understandable frustration.
Action item: Find out your estimate accuracy rate. Is it stagnant or improving over time? If you’re not seeing results, consider making a change.
POS collections pro-tip:
2. Deliver effective pre-service communications
One of the best ways to improve point-of-service collections is to put yourself in your patients’ shoes.
Most patients want to know what their care will cost prior to service, yet few talk about cost before their appointment. That’s a recipe for frustration.
In order to deliver effective pre-service communications:
- Consolidate and simplify information so it’s easy for patients to understand
- Preemptively answer frequently asked questions to prevent confusion later
- Deliver this information via the channel(s) they prefer — something that differs from patient to patient
Action item: Find out how your patients prefer to pay, and how they want to receive pre-service communications (phone, email, text, etc.). If their preferences don’t line up with your process, find a solution that does.
POS collections pro-tip:
3. Make paying easy with a powerful platform
Providers want to give patients a simple, streamlined payment experience. Yet 78% of providers can’t collect bills of $1,000+ in 30 days.
Why? Often, it’s because providers don’t make it easy for patients to get their questions answered and pay in a way that makes sense for them. They want to, of course, but the solutions they use aren’t supported by a platform that gives patients easy access to the information they want.
The best point-of-service collections tools will connect to a platform that:
- Allows patients to review their estimates on their own time
- Provides self-service support tools, such as secure messaging and live chat
- Offers multiple, affordable payment options that fit a patients’ budget
Action item: Find out how easy it is for patients to pay prior to service. Make sure your payment options include self-service digital payment.
POS collections pro-tip:
4. Give your team the tools they need
Compassionate communication is a powerful way to make sure patients understand what they owe and why. But a huge part of point-of-service collections is arming your team with tools they can trust.
In this case, put yourself in your staff’s shoes. It’s far easier to have a compassionate conversation if you know the patient received an accurate estimate. Furthermore, when staff has a single source of truth for everything from coverage to claim status, it makes them more confident and efficient.
To help staff collect faster, fuller amounts at the time of service, use a tool that:
- Pulls real-time eligibility data
- Generates accurate estimates
- Identifies patients that qualify for charity
- Determines a patient’s propensity-to-pay
- Automatically follows up on payment requests
Action item: Ask your staff to rate your current payment solution from 1-10. (Use an anonymous survey if needed.) If your results are lower than a 7, explore other tools.
Want to know more about Waystar’s Patient Payments?
Discover a better way forward.
Schedule a demo
Find this post helpful?
Learn how automation can boost staff satisfaction


