WAYSTAR AUTHORIZATION MANAGER
Eliminate delays.
Expedite approvals.
Prior authorization delays are the #1 cause of claim denials. Waystar’s Authorization Manager streamlines workflows, reduces manual work, and speeds up approvals — so patients get care faster.
Reduce denials + accelerate reimbursement
Prior authorization is the top revenue cycle bottleneck. RCM teams spend hours on the phone and payer portals, with delays impacting patient care and increasing costs.
Waystar automates the entire prior authorization process. No phone calls, no faxes — just approvals.
85%+
authorization auto-approval rate
Waystar data
TRUSTED BY HEALTHCARE LEADERS NATIONWIDE
Minimize rework.
Maximize results.
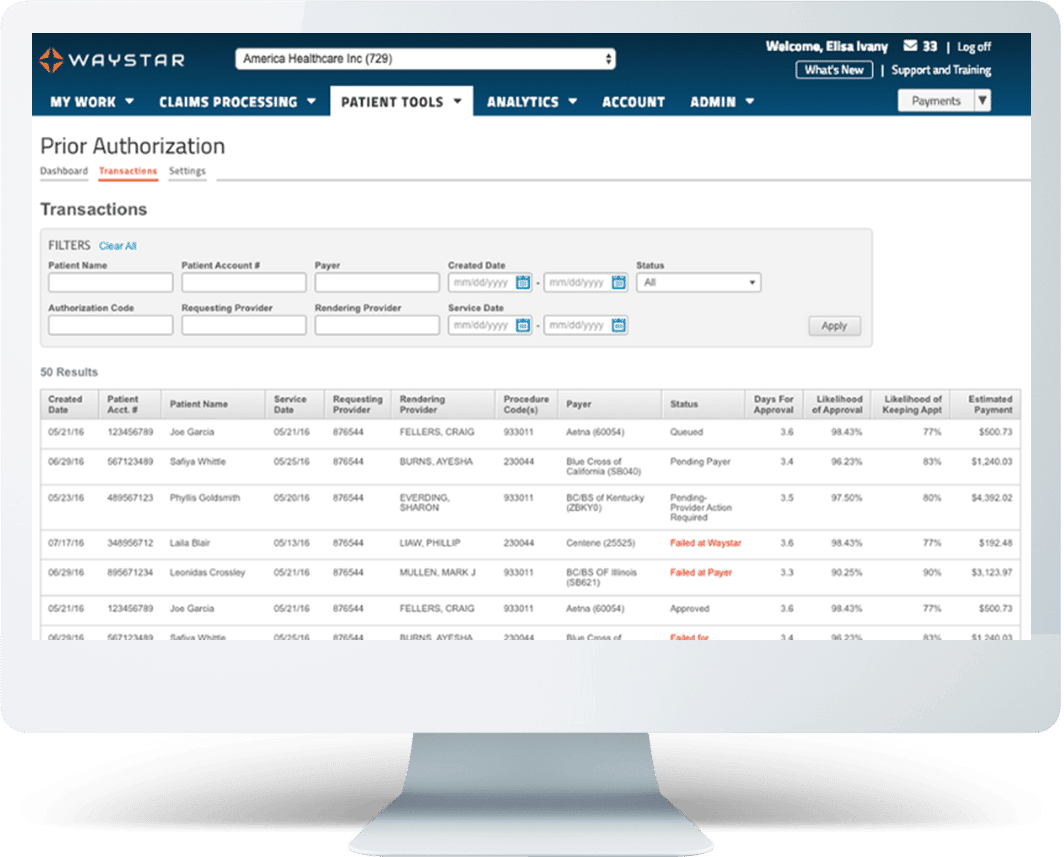
Waystar’s Authorization Manager uses advanced automation to help you increase speed and accuracy. Integrated in every authorization workflow, our advanced authorization verification instantly analyzes EHR, HIS, and PM orders, determining if an authorization is required and ensuring accurate submissions in real time. Forget about spending hours on the line or clicking through payer portals — the answers are delivered straight to you.
By The Numbers
50%+
Reduction in average authorization initiate time*
<2%
cancellation rate due to denied or delayed authorizations*
8-day
increase in average lead time*
97%
DAR clearance rate*
32M
authorization transactions annually**
30
service lines covered**
*Success story: Atlantic Health System, 2024
**Waystar data
Trending resources

Unlock Prior Authorization Potential
Explore Waystar’s prior authorization solution
Unlock a customized plan to see how Authorization Manager can help you improve efficiency and cut costs.






