Claim Management
The quick + clear path to fuller reimbursement
For providers of all kinds, managing claims is one of the most demanding parts of the revenue cycle due to deep-rooted manual processes, a lack of visibility into payer data, and other challenges.
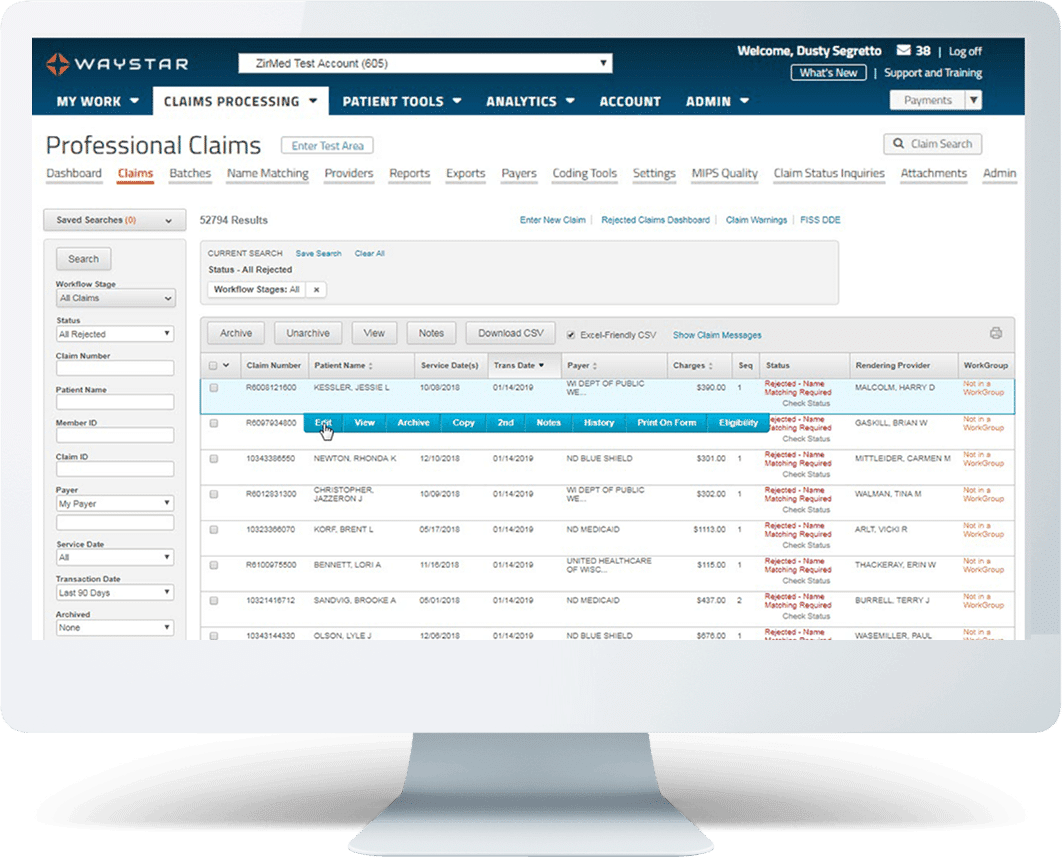
Things are different with Waystar. Our award-winning Claim Management suite can help your organization prevent rejections and denials before they happen, automate claim monitoring, and streamline attachments. What’s more, Waystar allows you to work both commercial and government claims in one place.
Request demo
Waystar Claim Management—by the numbers
TRUSTED BY HEALTHCARE LEADERS NATIONWIDE
“ We’re able to catch a lot of errors before our claims go out. When the claims go through Waystar, it results in a high clean claim rate, improving our efficiency and performance. ”

Explore our Claim Management solutions
Claim Manager | Claim Monitoring | Claim Attachments | Medicare Enterprise
Claim management resources
Take a deeper look at claim management
Below, we’ve compiled some tips and best practices surrounding claim management — and expert insights on how innovative technology can help your organization work smarter. Check out our resources below
A quicker path to more complete reimbursement
Claim status inquires: What’s at stake for your organization
Achieve claim management clarity with these 4 strategies
Save time and money by filing claims electronically

Talk with a Claim Management expert
Fill out the form below to have a Waystar expert get in touch. We look forward to speaking with you.