Today, healthcare denial management is not just a priority for RCM professionals — it is the priority.
“In recent surveys, three out of four respondents said reducing denials was their top priority,” said Christine Fontaine, Waystar Solution Strategist, in a recent denials webinar. “And 70% say claim management is more important now than it was pre-pandemic.”
Responses like this show that healthcare denial management is at a tipping point. Organizations are facing stress from every direction — regulations, population health, the economy — while continuously battling delays and denials. That creates wasted healthcare dollars that providers literally can’t afford amid narrowing (or even negative) margins.
“We understand why healthcare leaders believe denials are increasing — because they are,” says Christine. “Now, let’s dig a bit deeper into the top reasons denials actually happen.”
NOTE: Unless otherwise cited, data in this blog is from the 2023 Report: HFMA research + insights on denials in healthcare.
healthcare denial management pitfall:
1. Registration + eligibility
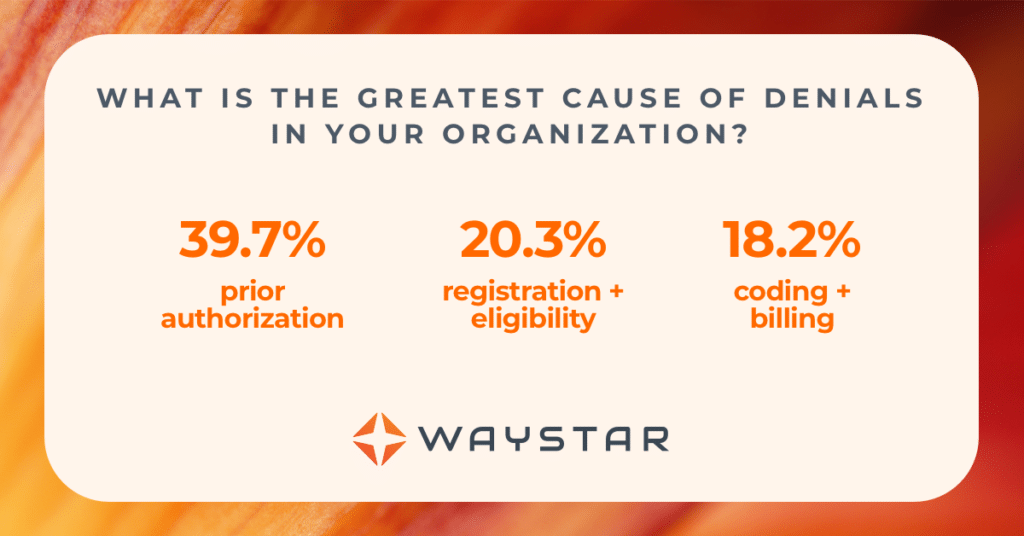
As always, registration and eligibility are top causes for denials. More than 20% of denials come from these two categories.
“What’s most burdensome is that of those denials, 55% are avoidable but yet non-recoverable,” says Christine. “That means more than half of frontend denials don’t have to happen — but once they do, that money is gone.”
The good news: denials related to registration and eligibility are showing consistent improvement. Why?
“Because providers are finally taking a hard look at process issues,” says Christine. “Technology is being embraced at scale — and not just technology, but purpose-built, intelligent technology.”

healthcare denial management pitfall:
2. Clinical validation
While registration and eligibility denials are beginning to level out, clinical validation denials are climbing. Medical necessity, for example, now comprises 8.1% of all denials.
That includes denials related to:
- Medical documentation
- Avoidable care
- Length of stay
- Level of care
- Lack of medical necessity (based on NCDs, LCDs, notice of non-coverage)
“What this data tells us is that we’re not doing a good enough job of validating what we’re ordering,” says Christine, “and that’s causing us to treat patients in non-covered ways.”
healthcare denial management pitfall:
3. Missing + invalid claim data
“I am shocked by the number of denials due to missing or invalid claim data,” says Christine. “These claims should get stopped by your EMR, which should also give you the ability to make powerful edits.”
If your EMR doesn’t have that capability, check your clearinghouse. At a minimum, they should be your safety net so you can be sure you’re stopping these sure-to-be-denied claims before they go out the door.
healthcare denial management pitfall:
4. Prior authorization
Prior authorization is (and will continue to be) problematic for providers. It is the top reasons for denials, causing a whopping 39.7%.
“Unfortunately, prior authorization is not going to get better; it’s going to get worse,” says Christine. “Payers want to ensure providers are only providing medically necessary services. Even Medicare now is being more proactive about prior authorization for certain exams.”
The result? A large number of first-pass denials that go nowhere.
“The reality is that, contractually, providers have agreed to do prior authorization for certain exams,” says Christine. “And if they don’t, they’ll get denied and have limited-to-no capabilities to overturn it. That will lead to them losing cash that’s crucial to the organization’s survival.”

The bottom line
With constantly changing rules, healthcare denial management will continue to grow — but your staff shouldn’t.
“Adding more staff isn’t the answer,” says Christine. “Bringing in people to triage your workload is a short-term fix, and one that will lead to burnout and turnover.”
Instead, focus on two things:
- Find an automated healthcare denial management system you can trust and
- Invest in training your staff to use it.
“If you don’t find the right solution — and offer your staff robust training and support when you do — you’re never going to fulfill your biggest responsibility: serving your patients.”
Want to learn more about healthcare denial management?
Download the survey by HFMA + Waystar.
Want to learn more about healthcare denial management solutions?