If you’ve ever had to chase down referral status from a payer, you know it’s a tedious, time-consuming process. Whether you’re calling payers or checking portals, referrals wreak havoc on efficiency — and they don’t stop there. If your organization routinely experiences delayed or extended referral processing, you risk everything from patient leakage to poor clinical outcomes.
Here are the basics of referral status, from the definition to the difference in referrals vs. authorizations.
What is a referral in healthcare?
A referral is an order from a primary care physician (PCP) that allows a patient to see and receive care from a specialist. PCPs use referrals when patients need:
- Expertise the PCP can’t provide
- Specialized treatment
- Further diagnostic testing or investigation
Most insurance payers require patients to get a referral before receiving care from anyone other than their PCP. If patients don’t get a referral first, the plan may not pay for the services.
What’s the difference in referrals vs. authorizations?
Although the term “referral” is often used interchangeably with “prior authorization,” they are not the same thing. While a prior authorization requests coverage for a medication, service, or treatment, a referral requests coverage for a specialist visit or for specialized medical service. And after you get a referral, further authorizations may still be required.
Think of it this way: A referral gets a patient in the door to see the specialist, but the next steps — certain medications, treatments, procedures — could still require the specialist to generate an authorization.

How do referrals work?
Once a PCP decides the patient needs to see a specialist:
- The PCP writes a referral
- The referral must be sent to the specialist AND
- The referral must be sent to the patient’s insurance provider
- The insurance provider must approve the referral
- The specialist can schedule care
- The patient can receive care under their benefits
Often, there’s a breakdown between steps 3, 4, and 5. Just like with prior auths, the referral must be approved by the insurer before the patient’s care can be covered. So, it’s crucial for healthcare staff to know which referrals have been accepted, rejected, denied, or need more information.
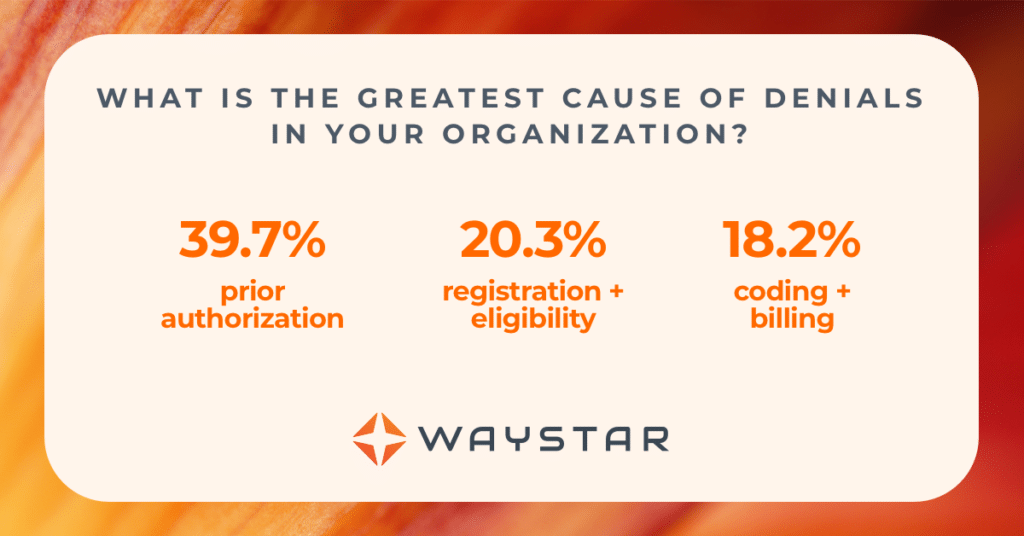
When everything runs smoothly, referrals and authorizations work together to ensure patients are cleared to get the care they need. However, front-end processes don’t always function seamlessly. In fact, a 2023 study by HFMA + Waystar showed that healthcare finance leaders believe 60% of denials can be attributed to the front end.
What problems can manually statusing referrals cause?
In the realm of healthcare referrals, approvals are everything. The insurance provider must approve a patient referral before care can be provided — or, more specifically, can be provided and covered, aka paid for. That second part is critical.
If a specialist visit or service happens before a referral is approved, the patient’s insurance provider may reject or deny that claim. This creates a huge problem for healthcare providers. Even if a referral simply needs more information to be approved, healthcare staff may not always know that — unless they can see the referral status. And that requires some digging.
Finding comprehensive referral details manually is error prone. It’s difficult to check a referral’s status by phone or online … then input that information flawlessly into your HIS or PM workflows … and to be sure all that information will be there exactly when other staff members need it.
What’s more, these tedious, time-consuming processes do more than just frustrate staff. They can also lead to:
- Delayed or canceled care
- Increased denials
- Poor patient experience
- Lost revenue + cash flow
How can automation help referral status?
As with any repetitive, manual process, automation is a powerful tool.
When you use software to check and deliver referral status directly into workflows, you can expedite the care path, minimize patient leakage, and create better clinical and financial outcomes for patients.
Benefits of automated referral status include:
- Streamlined workflows
- Improved staff efficiency
- A better patient experience
- Fewer denials
- Higher revenue capture
When choosing an automated referral status solution, look for a tool that:
- Centralizes all referral activities on one platform
- Checks status directly with the payer
- Retrieves comprehensive details about referral status
- Delivers that information seamlessly into your workflow
Want to know more about Waystar Referral Status?
Waystar’s Referral Status in the Authorization suite uses API and EDI technology to status referrals directly with the payer, and it automatically updates work queues accordingly.
The solution’s timely responses:
- Minimize the errors and delays that cause denials
- Help teams schedule patient follow up promptly
- Speed authorization referral closure