Claim Manager
Cleaner claims. Fewer denials.
Claim management software is one of the biggest investments for your healthcare organization, and making the right decision is critical to see high returns and powerful results. As part of a unified healthcare payments platform, Waystar’s Claim Manager offers intelligent AI capabilities, advanced automation, and data to streamline your workflows, reduce the cost-to-collect, and bring in revenue — faster and more easily.
To overcome ever-increasing complexity in today’s healthcare environment, Waystar’s software platform offers one, seamless solution for claim types across payers — and integrates with 530+ HIS and PM systems to support your healthcare organization’s needs.
Request demo
98.5%+
average clean claim rate
Source: Waystar data
Waystar Claim Management by the numbers
What makes Waystar Claim Manager different
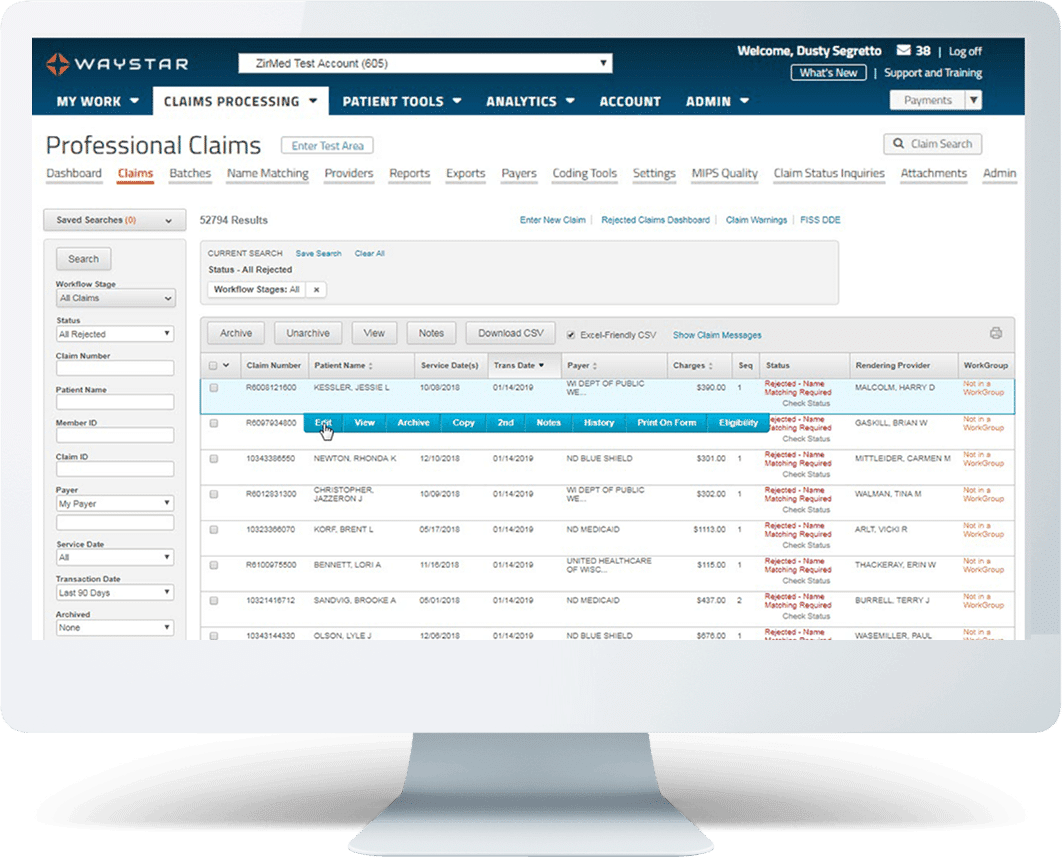
Get your claim right, the first time
Gain greater visibility into and more control of your claims with highly customized technology that produces cleaner claims, prevents denials, intelligently triages payer responses, and makes custom claim rule creation a breeze. Waystar Claim Manager improves operational efficiency and accuracy with advanced automation, minimizing manual effort and allowing staff to focus on higher-value tasks.
Features + Benefits
- Get claims right the first time with precise claim edits for the right payers using configurable rules and crowdsourced insights
- Waystar’s Rule Manager allows custom rule creation in minutes, now enhanced with AltitudeAssist™ for generative AI-powered precision and speed
- Automated Eligibility Verification + Coverage Detection integration helps prevent eligibility denials by ensuring accurate coverage data prior to claim submission
- Flexible claim search options allow staff to easily find and review claims
- Simple rejection messaging removes the cumbersome task of interpreting payer responses
- Quickly and easily complete enrollments with eSignature and enrollment services
- Waystar’s Automation Intelligence Center provides a clear view of automation and AltitudeAI™ features available for workflow optimization
AI INNOVATION IN CLAIM MANAGEMENT
Maximize efficiency with AI
Waystar’s Rule Manager solution leverages Waystar AltitudeAI™’s powerful generative AI capabilities that create custom claim edits with ease. This innovative tool can automatically fix issues before claim submission, helping to prevent more denials upfront for faster, fuller reimbursement.
3mins
Cut custom claim edit creation from 3 days to approximately 3 minutes
TRUSTED BY HEALTHCARE LEADERS NATIONWIDE
Claim Management Implementation
Switching to Waystar is easy — and it’s worth it
We know you can’t afford cash or workflow disruptions. That’s why Waystar works hard to make enrollment easy and seamless, and why we’ve invested in in-house implementation and support experts with decades of experience. We’ll be with you every step of the way, customizing workflows to fit your needs and preferences, whether you’d like to work in your HIS or PM system or in the Waystar interface. Find out why our clients rate us so highly.
Claim Manager resources
Success that speaks for itself
For years, we’ve helped clients increase efficiency and collect payments faster and more cost-effectively. Check out the success stories below to see just a few examples.
Health Care & Nursing Services

Access a world of possibility in one platform
When you work with Waystar, you get more than just a top-rated clearinghouse and expert support. You get access to an end-to-end software platform that can automate and streamline your entire revenue cycle, give you insights into your operations, and more. Explore the solutions that complement Claim Manager to help you get even better results:
Take the next step to see measurable revenue cycle results
Switching revenue cycle partners can be daunting. But with Waystar’s white-glove client support and innovative, user-friendly software — it’s worth it. Reach out to an expert below to see how your healthcare organization can reach peak performance.