
Partnering for powerful results
Waystar + eClinicalWorks

Waystar seamlessly integrates with your eClinicalWorks system to simplify healthcare payments so you can focus on your patients. Designed especially for eClinicalWorks practices, our smart platform helps practices streamline revenue cycle workflows, enhance productivity, and bring in more revenue — faster and with less work.
Imagine easier eligibility verification. What about denial management that helps you prevent denials up front? Or claim monitoring that saves your staff time to focus on what really matters? It’s all possible with the right combination of automation and AI — not to mention excellent client support.
With 20+ years of experience in healthcare revenue cycle, Waystar is known for simplifying healthcare payments for providers like you. And with 18+ years working with eClinicalWorks, we’re ready to be the proven partner you need.
Waystar + eClinicalWorks by the numbers
34k+
shared providers
3K+
practices
98.5%
Waystar clean claim rate
18
years of partnership
Advanced bundle designed with practices in mind
You’ve chosen eClinicalWorks for its market-leading practice management system, but are you making the most of it? Waystar offers multiple RCM bundles including an advanced bundle to help you get exactly what you need, whether you’re looking to automate denials, appeals, and coverage detection. Set it and forget it when it comes to claim status checks. And even predict a patient’s likelihood to pay. Know what’s even better? It all works from inside eClinicalWorks.
Discover the way to...
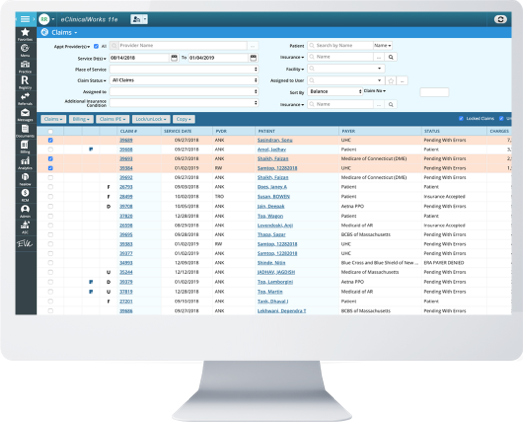
Simplify claim management
With costs rising alongside the pressure to collect, you need to get the most out of your RCM software. Waystar integrates with your existing eCW solution to accurately automate claim monitoring, simplify AR workflows, decrease rejections, streamline attachments — and collect faster and fuller reimbursement.
Prevent + prioritize denials
Oversized workloads and obsolete denial processing mean you’re probably leaving a lot of revenue on the table. You’re not alone. The majority of denials that are recoverable are never reworked. But with eCW and Waystar, you can save time and money. Our solution helps you prevent and prioritize denials, automate appeals, and capture more revenue.
Find hidden coverage
When coverage isn’t provided by your patients, looking for it is quite an undertaking. But finding hidden coverage can be fast and efficient when you integrate your eCW platform with Waystar. Take advantage of our industry-leading claims database and robust payer connections to generate more cash flow and relieve financial burdens on patients.
The easy way to convert EOBs
Ready to eliminate data-entry errors that create unnecessary work? When your staff uses Waystar's EOB conversion within eCW to reconcile and post payments, you'll streamline workflows, increase transparency, and get time back to focus on higher value tasks — like giving your patients the best financial experience possible.
Choose an experience that puts people first
Lighting your way forward today + in the future
Waystar is a technology company that serves people — and we always remember that. Whether you are implementing new solutions, seeking fresh strategies for success, or simply need better support, we ensure it’s easy to get answers when you need them most.
96%
same-day support case resolution1
11s
average time to reach live support1
74+
client NPS2
5K+
support articles & training guides
- Waystar data, 2023
- NPS survey, 2023
Recognized for excellence





“ Not only does Waystar seamlessly interface with eClinicalWorks, it offers opportunities to sharpen our processes for eligibility verification, claims submission, and remittance. ”

A platform designed with providers like you in mind
Waystar and eClinicalWorks have been preferred partners since 2005 and in that time we’ve helped many practices enhance their bottom line. Check out our case studies to learn more.

ROCKFORD ORTHOPEDICS
38%
decrease in rejections
11,000+
monthly claims submitted
37%
increase in staff productivity
Waystar + eClinicalworks
The way forward starts here
With our smart, integrated platform powering revenue cycle processes behind the scenes, you can reach new heights in healthcare. Speak to a Waystar expert.