Resources
Whether you’re looking for a specific case study or just exploring, you’ll find all the resources you need on this page.
Case Study
Transformations Care Network
A mental healthcare network’s journey to improve claim visibility + reduce denials
Case Study
Prosthetics & Orthotics Group
How Waystar enabled Prosthetics & Orthotics Group to reduce denials, implement analytics and streamline billing operations.
Case Study
Nemours Children’s Health
A pediatric health system’s journey to streamline claims + patient payments
eBook
The ROI of AI in healthcare payments: Which metrics matter?
This eBook reveals the metrics that leading healthcare organizations track to prevent denials, accelerate appeals, and ultimately collect more revenue. Uncover the specific KPIs you need to define — and achieve — success, from cost-to-collect to denial rate.
Guide
AI in healthcare definitions explained: A glossary for revenue cycle leaders
The healthcare industry’s increasing dependence on artificial intelligence (AI) means new terminology is constantly evolving, making it challenging to keep pace. This essential guide is designed specifically for revenue cycle leaders, cutting through the complexity to provide clear, easy-to-grasp definitions of critical AI concepts.
Case Study
ProScan Imaging
A radiology network’s journey to reduce denials + improve collections
Case Study
MedQuest Associates
An outpatient diagnostic imaging organization’s journey to streamline claim management
Fact Sheet
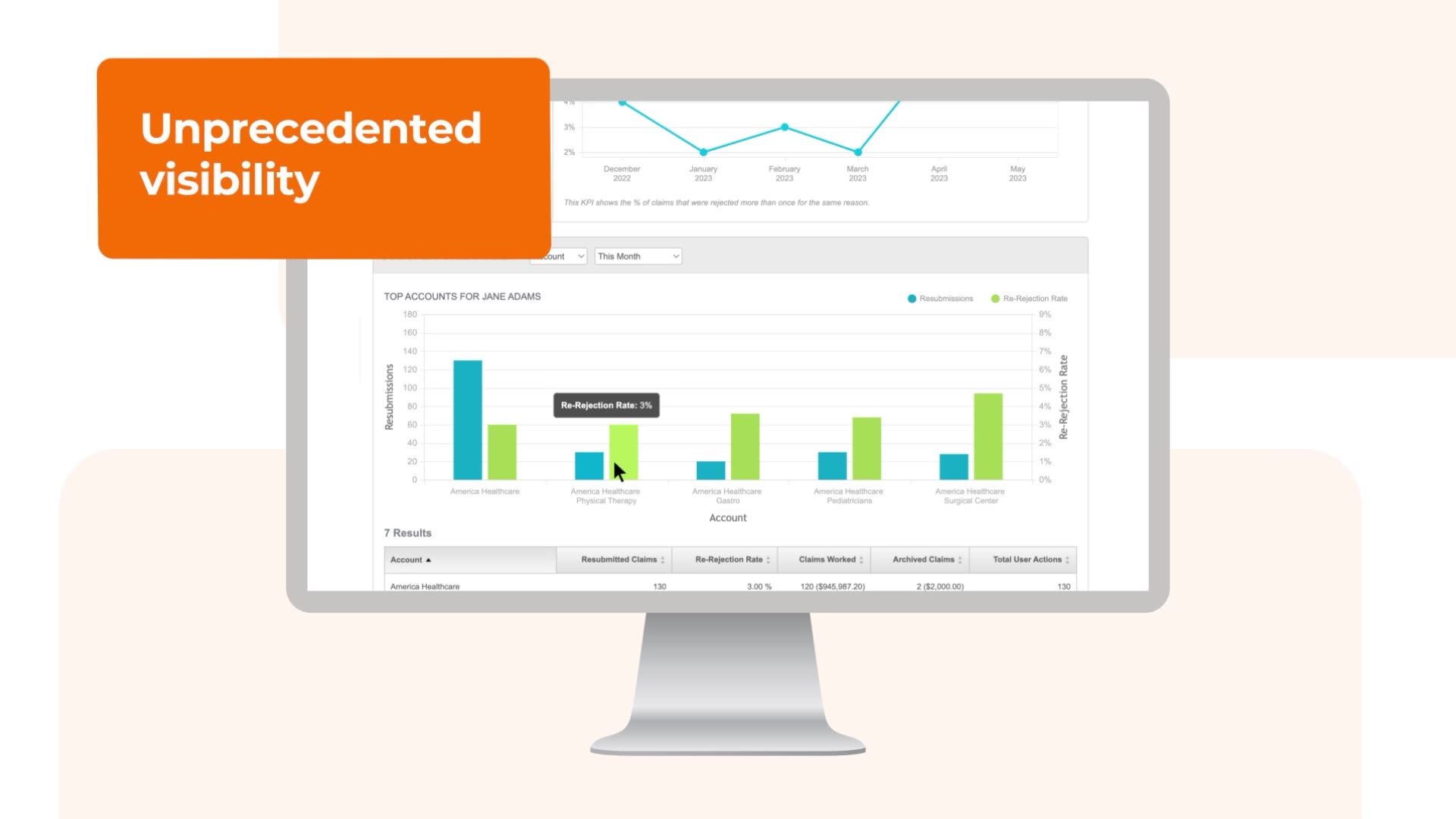
Claim Manager Peak
Waystar’s Claim Manager Peak offers the AI-powered automation you need to lower cost-to-collect and get faster, fuller payments.
Case Study
Advent Health
A health system’s journey to redesign reconciliation + realize more revenue
Fact Sheet
Simplify NOE Submission
Tight deadlines and delays in processing can result in penalties or non-reimbursement for late submission while limited transparency into the status of NOE submissions makes troubleshooting difficult. These challenges are causing more hospice providers to turn to Waystar to submit NOEs quickly and easily.
Fact Sheet
AltitudeAI
Waystar AltitudeAI™ is purpose-built to automate work, prioritize tasks, and eliminate errors. Pervasive across the end-to-end software platform, our AI solutions drive efficiency and yield meaningful results for healthcare providers.