SIMPLIFY HEALTHCARE PAYMENTS
The Waystar
Innovation Lab™
Explore breakthrough AI and advanced automation designed to simplify workflows, eliminate errors, and accelerate revenue — transforming processes for healthcare revenue cycle teams nationwide.
SPRING 2025
Waystar Innovation Showcase
Watch the full Waystar Innovation Showcase and hear directly from our revenue cycle experts about the AI-powered capabilities and advanced automation cutting end-to-end RCM complexity.
INNOVATIONS TO OVERCOME RCM CHALLENGES
Prevent denials + streamline appeals
Discover how Waystar’s platform automates denial prevention by catching critical claim errors before they reach the payer and effortlessly generating appeal letters using generative AI.
Accelerate payments + strengthen financial health
Speed cash flow with generative AI and advanced automation for insurance verification, coverage detection, and prior authorizations — reducing denials, increasing collections, and boosting financial performance from the start.
Enhance the patient financial experience
Leverage the power of smart software to meet patients where they are — online, on the go, on their schedule — and tailor their financial experience based on behavior-based preferences.
Financial Clearance
Speak to an expert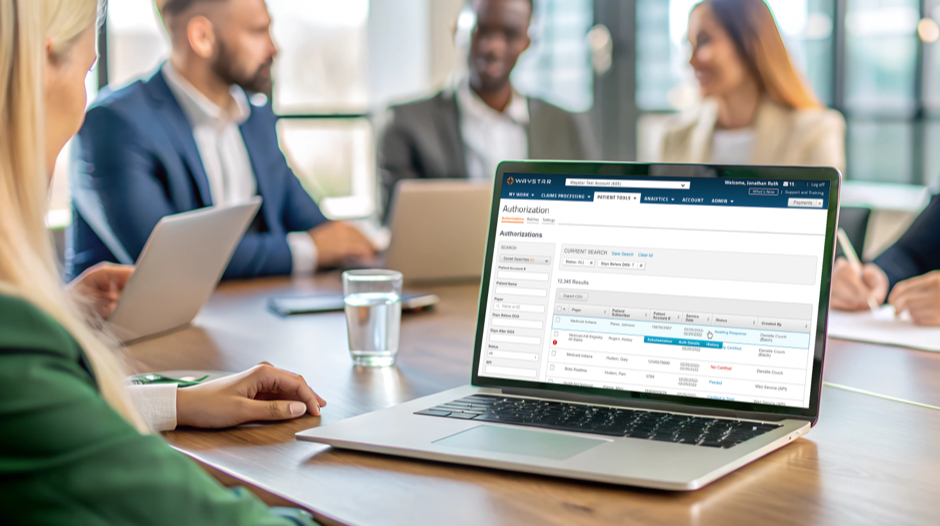
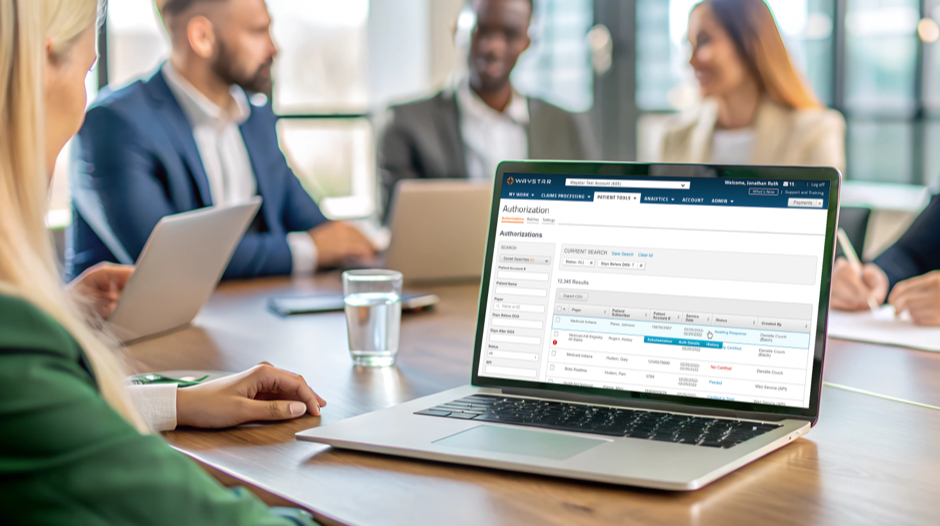
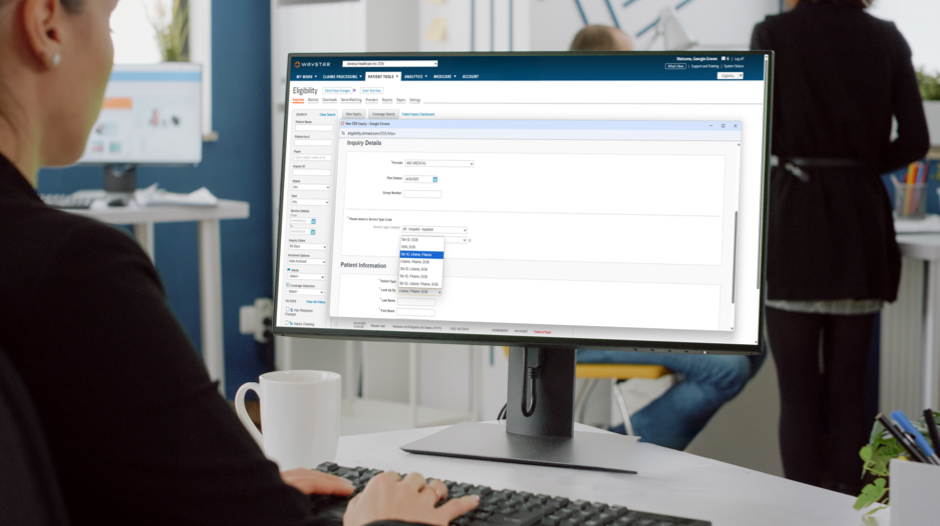

32M
authorization transactions annually
1.2K
payer connections for eligibility
30-40%
average Coverage Detection hit rate
Waystar data
Patient Financial Care
Get in touch
20-30%
average collections lift
60-80%
average self-service pay rate
61+
patient NPS
Waystar data
Revenue Capture
Request a demo

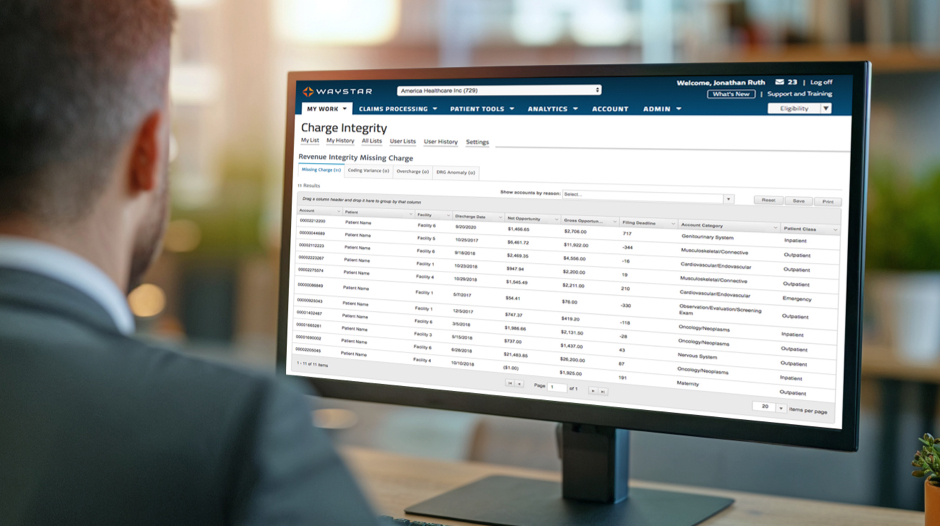
4:1
average ROI for Charge Integrity
$8K
average DRG Anomaly claim recovery
95%
Waystar auditor agreement rates for Charge Integrity + DRG Anomaly
Waystar data
Claim + Payer Payment Management
Connect with an expert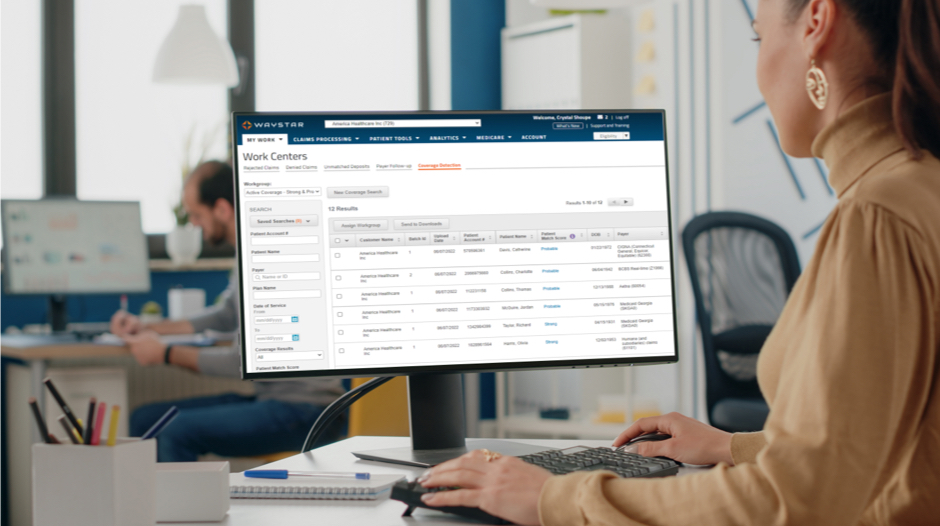
2.5M+
continuously updated edits
5K+
payer connections
98.5%
first-pass clean claim rate
Waystar data
Denial Prevention + Recovery
See it in action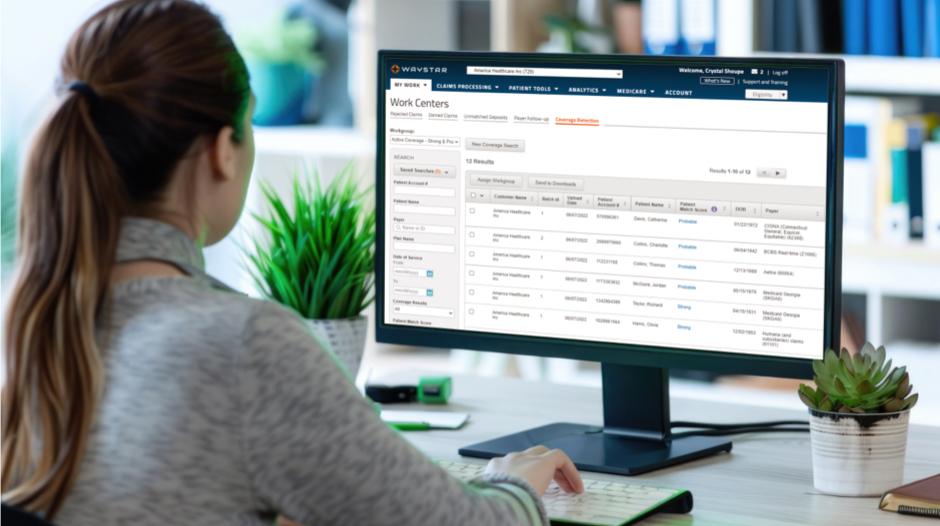
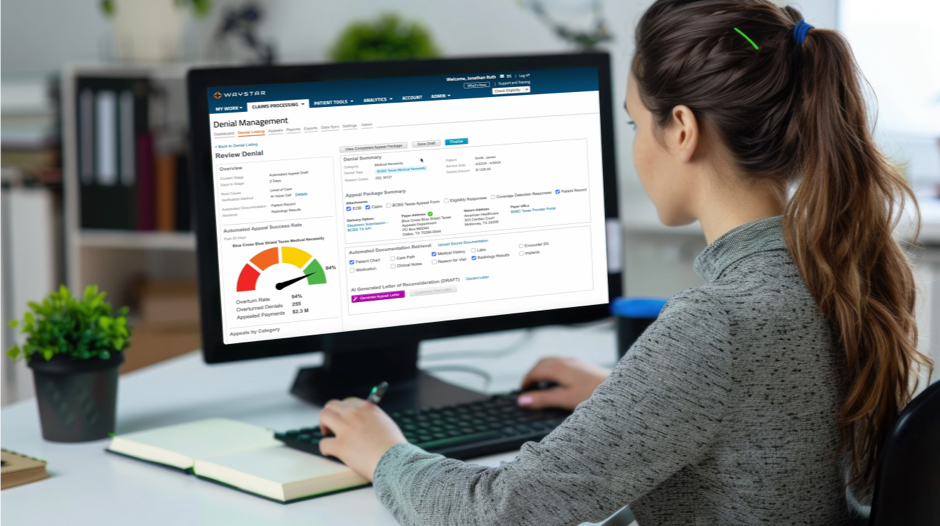
3X
Faster appeal package creation with AltitudeCreate™
16mins
time savings per appeal package with AltitudeCreate™
100%
paperless appeals process
Waystar data
Analytics + Reporting
Book a demo


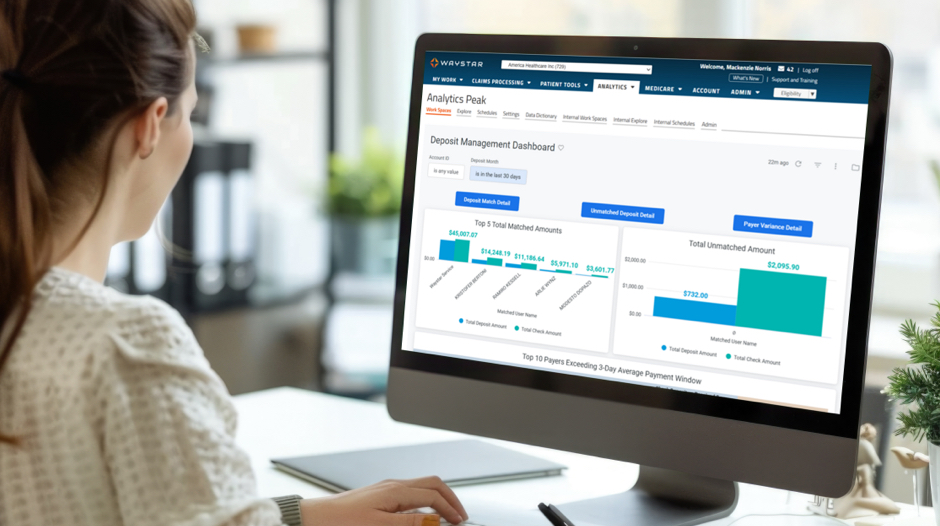
145+
pre-built KPIs for claims, remits + denials
35+
pre-built revenue cycle specific reports
12
pre-built analytics dashboards for Pro + Peak
Waystar data
LEADING THE WAY IN INNOVATION
innovation1
effectiveness1
ease of use1
1Waystar vs. Competitors, Qualtrics survey (2025)
INNOVATION IN ACTION
Trending resources
Speak to a Waystar expert
Curious to learn more about Waystar’s cutting-edge innovations? Reach out to speak with a Waystar expert to learn how these advancements can help your healthcare organization see powerful results.