Resources
Whether you’re looking for a specific case study or just exploring, you’ll find all the resources you need on this page.
Case Study
MedQuest Associates
An outpatient diagnostic imaging organization’s journey to streamline claim management
Fact Sheet
Claim Manager Peak
Waystar’s Claim Manager Peak offers the AI-powered automation you need to lower cost-to-collect and get faster, fuller payments.
Case Study
Advent Health
A health system’s journey to redesign reconciliation + realize more revenue
Fact Sheet
Simplify NOE Submission
Tight deadlines and delays in processing can result in penalties or non-reimbursement for late submission while limited transparency into the status of NOE submissions makes troubleshooting difficult. These challenges are causing more hospice providers to turn to Waystar to submit NOEs quickly and easily.
Fact Sheet
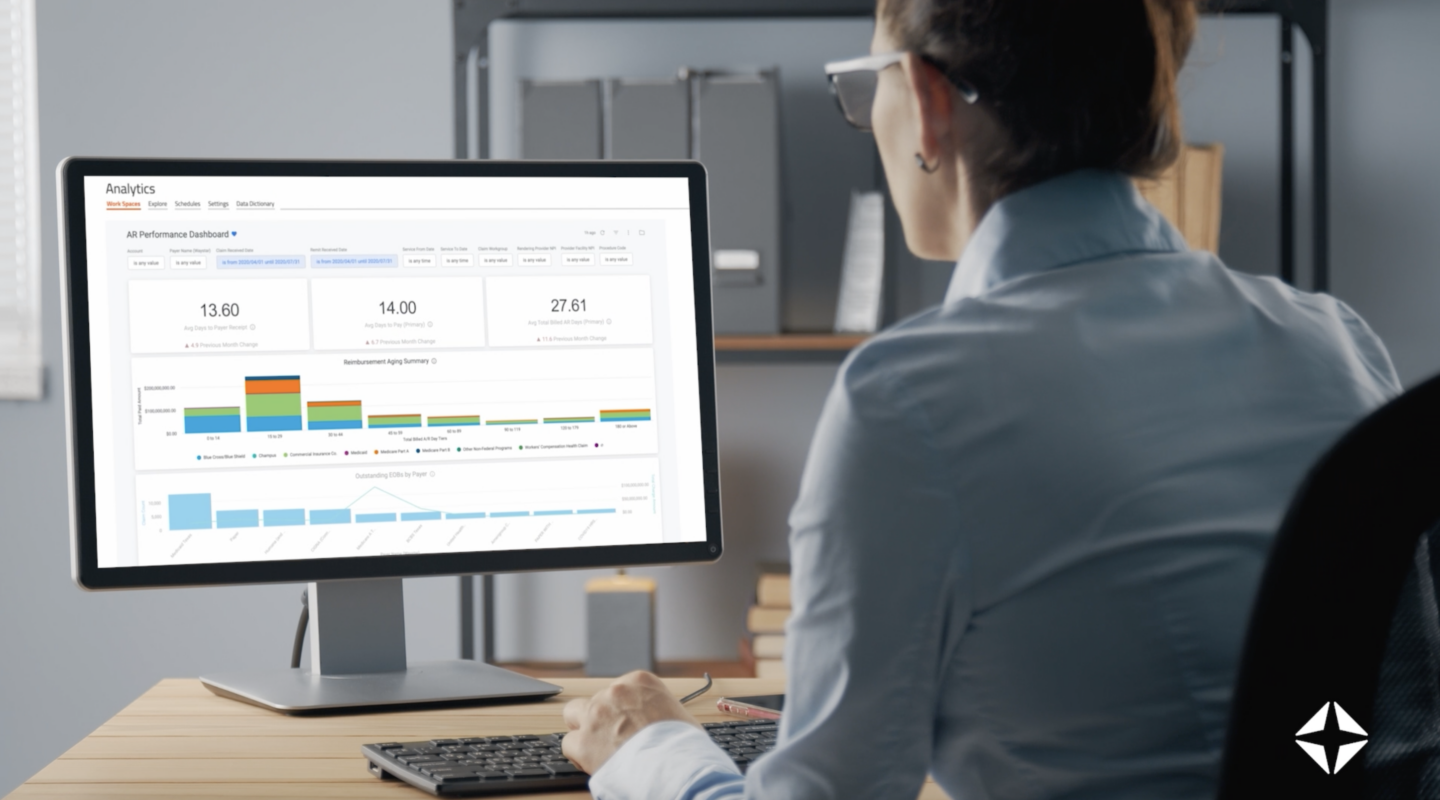
AltitudeAI
Waystar AltitudeAI™ is purpose-built to automate work, prioritize tasks, and eliminate errors. Pervasive across the end-to-end software platform, our AI solutions drive efficiency and yield meaningful results for healthcare providers.
Fact Sheet
Auto Eligibility + Auto Coverage Detection
To get claims right and prevent more denials upfront, you must integrate AI, automation, and robust data into your revenue cycle. Waystar gives you what you need to prevent more denials — with less effort.
Case Study
Preferred Home Health Care & Services
Home healthcare organization streamlines claim management + enhances efficiency
Report
Examining AI adoption + ROI in healthcare payments
Waystar partnered with Modern Healthcare to conduct a research study into the importance of AI in revenue cycle management software today.
Case Study
Ortho Illinois
Orthopedic healthcare provider enhances claim management + revenue cycle efficiency
Case Study
Austin Radiological Association
Radiology practice enhances claim management + the patient financial experience
eBook
Achieve claim management clarity with these 4 strategies
Unlock clean claims, fewer denials + faster, fuller payments.
Fact Sheet
EOB Conversion
Waystar removes the manual, error-prone process of posting paper EOBs — helping you lower costs and reclaim staff time.
Case Study
in2itive Business Solutions
Billing services provider simplifies claim management + boosts efficiency
Fact Sheet
EOB Conversion + Payer Lockbox
Waystar’s Remit Manager provides one simple platform for all payer payments, increasing efficiency, visibility, and accuracy.
Fact Sheet
Claim Attachments
Waystar’s Claim Attachments solution streamlines claim attachment workflows — increasing efficiency, improving cash flow, and avoiding costly AR delays.