The state of claim status inquiries today
Are you manually managing claim status inquiries or only partially electronically? That is, are you picking up the phone and dialing payers’ automated lines, visiting their outdated web portals, or sending mail or faxes? If so, you’re certainly not alone.
According to the 2018 Coalition for Affordable Quality Healthcare Index, in 2018, approximately 737M claim status inquiries were transmitted in one of the ways above.1
What’s at stake for your organization
Manual claim monitoring places tremendous strain on hospitals and practices’ billing teams, who are already stretched thin. Here are the top five challenges organizations face with manual claim status checks:
- Manual inquiries take considerable time and resources.
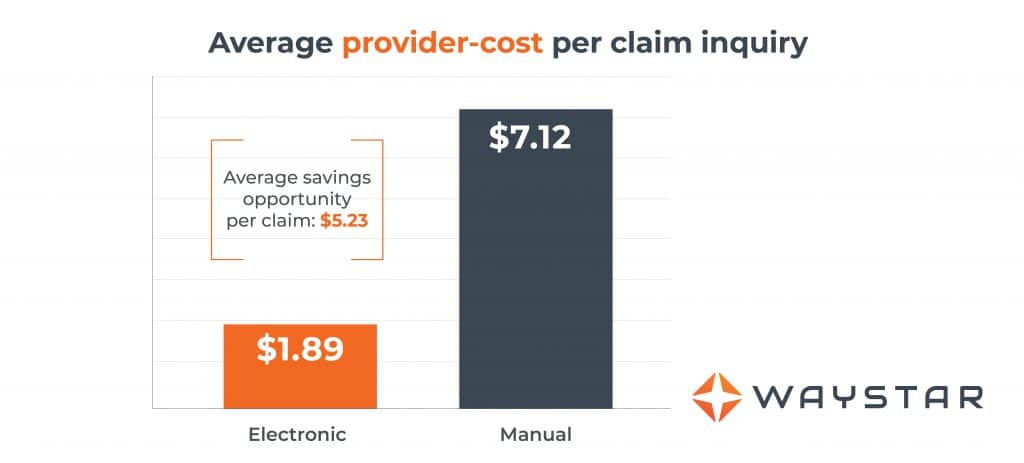
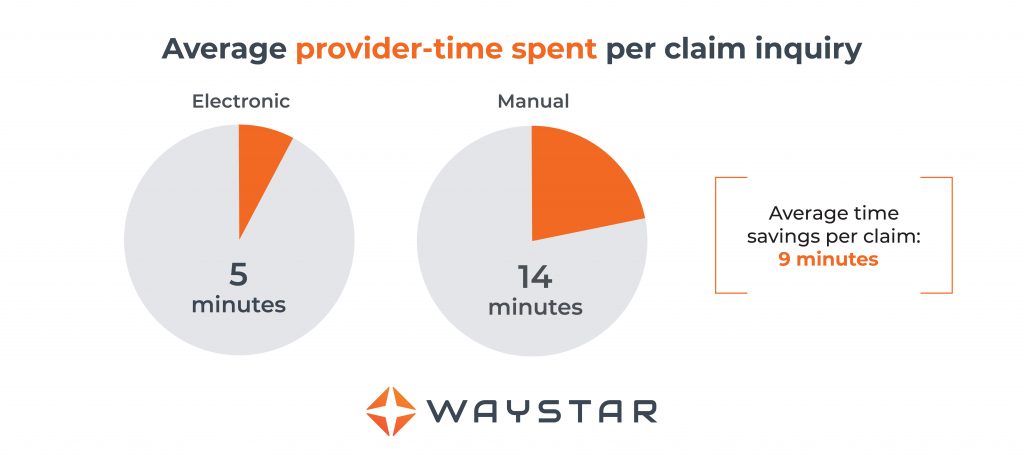
CAQH found that each time a provider manually contacts a payer to check the status of a claim, the process, on average, takes 14 minutes and costs providers $7.12.2 And, that estimate only takes the cost of labor into account; it doesn’t consider overhead or transactional costs, or the opportunity costs of taking staff away from other, higher-value RCM tasks. - Many claim status inquiries don’t produce actionable results.
- Payers often limit the number of inquiries that can be placed during each call.
- It’s difficult to gain visibility into claims and prioritize high-yield accounts.
- PM systems and HIS must be manually updated by FTEs following any inquiry.
Throw in the fact that more than 20M new patients have entered the U.S. healthcare system in the last few years and the need for smarter claim management is more important than ever.3
A smarter way to work: the beauty of automation
Claim status monitoring presents the highest annual savings opportunity of any administrative task CAQH explores in its index. With full adoption of electronic claim inquiries, the “annual savings potential for the medical industry is as much as $2.6B.”4
More and more providers across the spectrum of care are recognizing the value of automated claim monitoring and are incorporating it into their greater claim management strategy.
In 2013, adoption of electronic claim status inquiries was at 48%. By the end of last year, it had risen to 71%.5 When you consider the financial and operational upside of automated, electronic monitoring, it’s easy to see why.
What you stand to gain: by the numbers
Finding the right fit
Not all automation solutions are equal. You’ll want to choose the tech that offers the effectiveness and flexibility your organization needs.
A claims status inquiry solution should:
- Automate status checks and report valid, accurate information
- Provide a mechanism to work by exception, so your team can focus only on claims that need attention
- Translate status information into consistent, plain English messages to boost your team’s productivity
We hope this piece has shed some light on the inefficiencies of manual claim status inquiries — and the time and cost savings you stand to gain by implementing the right automated claims monitoring solution. For more information on this pivotal RCM topic, check out this brief guide.
Sources:
1, 2, 4, 5 “2018 CAQH Index: A Report of Healthcare Industry Adoption of Electronic Business Transactions and Cost Savings” https://www.caqh.org/sites/default/files/explorations/index/report/2018-index-report.pdf
3 “Since Obamacare Became Law, 20 Million More Americans Have Gained Health Insurance,” Fortune, Nov. 15 2018
http://fortune.com/2018/11/15/obamacare-americans-with-health-insurance-uninsured/


