In an industry overwhelmed by administrative complexity and rising costs, healthcare leaders are finding game-changing value in artificial intelligence (AI). A new study by Forrester Consulting, commissioned by Waystar, confirms it: healthcare payment AI is no longer experimental — it’s essential.
In the study, 82% of leaders agree that AI is an integral part of their organization’s revenue cycle management (RCM). From automating manual processes and improving accuracy to suggesting smarter financial decisions, here are some of the key findings from the research.
From hype to impact: AI delivers double-digit gains in healthcare payments
Healthcare organizations that have embraced AI in healthcare payments are reporting real gains. Across critical areas like claim follow-up, payment accuracy, denial prevention, and workforce efficiency, organizations saw improvements ranging from 13% to 37%.
Specifically, AI-powered improvements include:
- 13% claim follow-up
- 18% payment accuracy
- 21% faster payer payments
- 22% cash flow
- 23% visibility in reporting and analytics
- 27% denial prevention
- 36% workforce efficiency
- 37% patient financial experience and collections
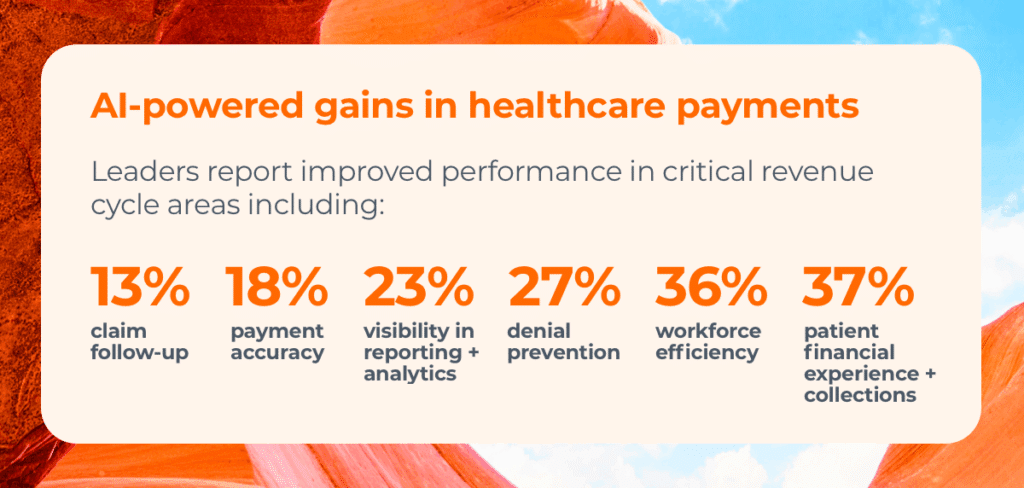
These aren’t marginal upgrades — they’re meaningful shifts. Surveyed decision-makers said their teams now rely on AI to minimize manual labor, improve transaction speed, and unlock time for more strategic work.
One standout area? Predictive analytics. The ability of AI to forecast payment issues, flag high-risk claims, and optimize denial management is transforming how providers approach RCM decision-making.
Trust in healthcare payments AI is growing — and so are investments
Initial skepticism about AI’s role in healthcare is subsiding. A full 60% of leaders say they trust AI more than they did when starting implementation — and 18% aren’t concerned about the integrity of the output at all.
With confidence comes investment. Of the surveyed organizations:
- 70% view AI as a top priority in revenue cycle management, and
- Nearly 60% plan to increase spending over the next two years.
What’s fueling that momentum?
- Denial prevention
More than half of respondents (56%) cite denial prevention as the top benefit of AI, with average improvements of 27%. - Accuracy + speed
From faster eligibility checks to more accurate coding, healthcare payment AI is streamlining processes at a previously unattainable rate. - Cost savings
AI is cutting administrative waste — a $350 billion a year problem in healthcare RCM — which frees up staff to take on highly skilled tasks or return to patient care.
Waystar clients are already using AI + generative AI to prioritize the denials most likely to be overturned, autonomously generate appeal letters, and more.
Organizations plan to maximize the impact of AI investments — and avoid the pitfalls
With continued plans to invest in AI, leaders have two overarching goals: (1) to ensure every investment has a measurable impact, and (2) avoid the challenges they faced with AI the first time around.
To maximize payoff + prevent problems, leaders plan to:
- Partner with trusted vendors
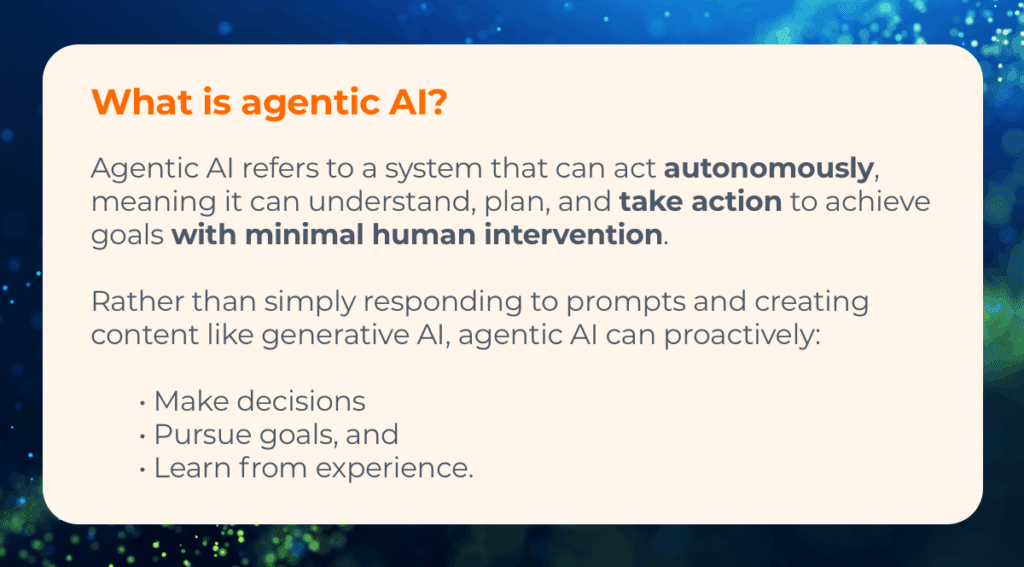
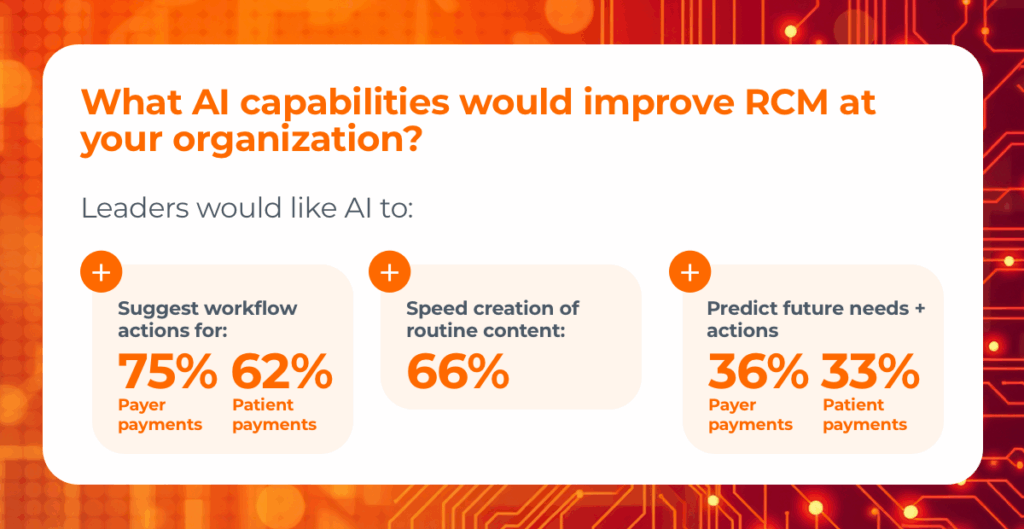
Implementing AI is especially challenging if the process isn’t well managed. That’s why most organizations plan to partner with a current vendor they already trust. That way, they can build on existing solutions and data, realize value sooner, and rely on proven technology to deliver results. - Apply AI to payer-facing interactions
When asked what new AI capabilities they want, payer-related outcomes top the list. Leaders want agentic and generative AI tools that will improve key metrics such as claim rejection rate, net collection rate, and cost-to-collect. - Foster greater internal collaboration
Uncertainty about which processes merit AI investment has been a huge hurdle for many organizations. Now, 82% coordinate AI strategy between IT and RCM leaders from the start to ensure their investment aligns with key business goals.
This strategic approach maximizes ROI and supports smarter uses of predictive analytics — enabling teams to act on insights rather than just react to data.
Looking ahead: 3 research-backed steps to take with AI in healthcare payments
For healthcare organizations still charting their AI journey, the research offers three key takeaways:
1. Define clear use cases
Identify where healthcare payment AI can deliver value, including:
- Which revenue cycle tasks AI will support
- The expected benefits
- How you’ll oversee the process
This clarity will help you build realistic timelines and prioritize high-impact opportunities.
2. Build trust through wins
Deploy AI in targeted areas tied to top investment drivers first — denial prevention, workforce efficiency, visibility In analytics, etc.
Seeing real, incremental progress in key areas will build internal confidence while delivering value. That will pave the way for broader AI adoption.
3. Empower your workforce
Train staff to use AI tools effectively — not just technically, but ethically and securely — as they shift from routine tasks to strategic roles. And be sure to reexamine revenue cycle workflows that were originally designed for humans to ensure everyone is aligned in terms of new responsibilities, technologies, and incentives.
Waystar clients often participate in our Early Adopter Program, which leverages generative AI to help them hit metrics like a 90% accuracy rate in authorizations..See how to join here.