Waystar’s Denial Prevention + Recovery suite empowers organizations like OOMC, U.S. Digestive Health, and Spectrum Eye Care to improve appeal success rates and bring in faster, fuller payments. It’s all possible with Waystar’s innovative Denial + Appeal Management solutions leveraging generative AI, automation, comprehensive data sets, and predictive analytics.
With Waystar Denial + Appeal Management, you’ll harness:
- AI + predictive analytics to prioritize the denials most likely to be overturned and paid leveraging AltitudeAI™
- Autonomously generate appeal letters using generative AI powered by AltitudeAI™
- A 100% paperless process + batch appeal submission options to increase efficiency
- Appeal tracking + proof of delivery to eliminate uncertainty
- Customized, exception-based workflows to meet your unique needs
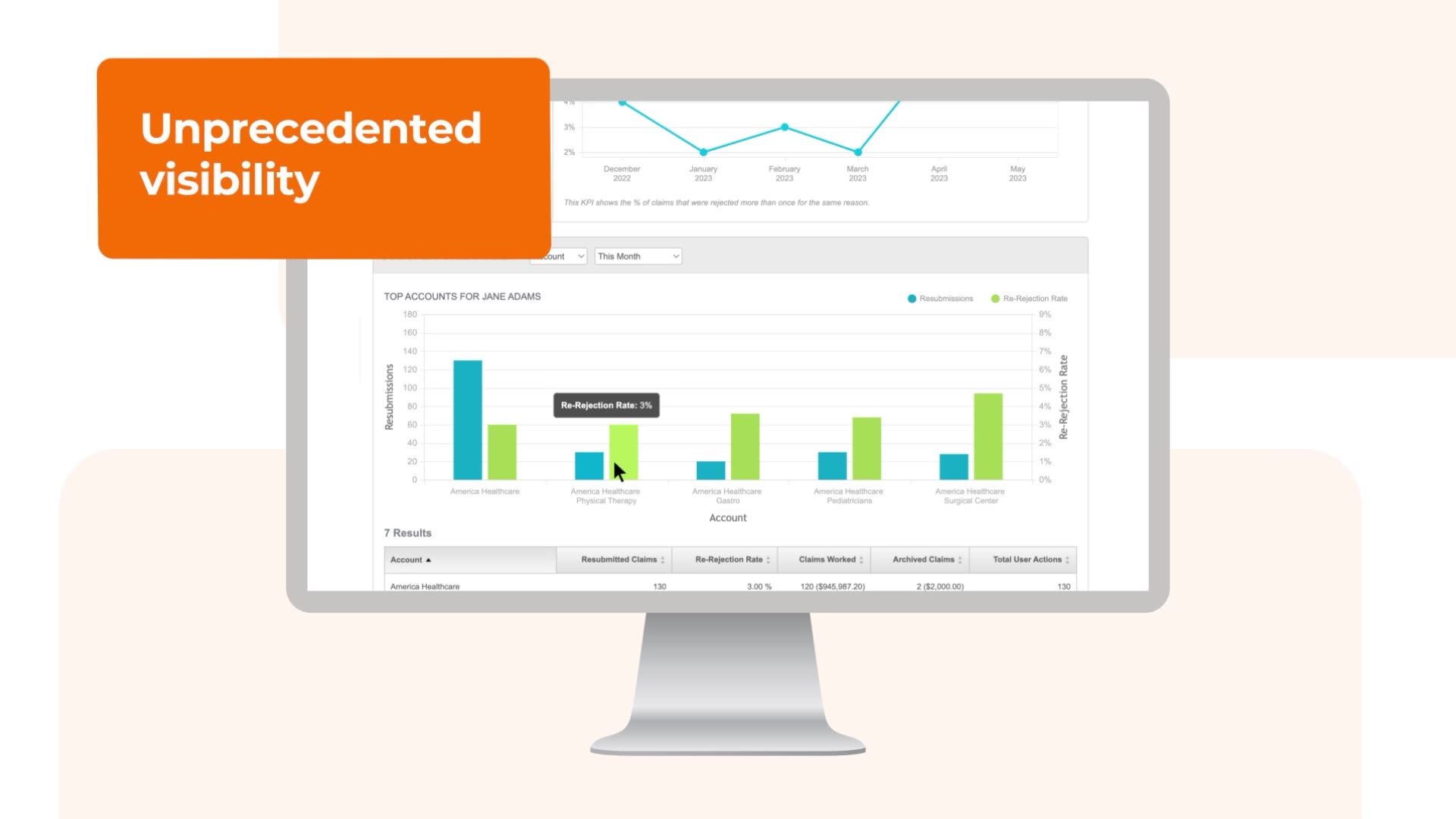
- Advanced analytics + root-cause reporting to support decision-making and denial prevention
- Automatically verify and identify updated coverage information for eligibility-related denials using Auto Coverage Detection, accelerating collections and reducing denial follow-up