Managing claims is one of the most demanding parts of the revenue cycle due to deep-rooted manual processes, a lack of visibility into payer data, and other challenges. For provider organizations — like U.S. Digestive Health, EyeSouth Partners, and Gastro Health — Waystar’s award-winning Claim + Payer Payment Management solutions prevent rejections and denials before they happen, automate claim monitoring, and streamline attachments.
With Waystar’s Claim Management solutions, billing teams harness:
- Easy-to-understand “How to fix” messages to simplify confusing payer responses
- eSignature and enrollment services to simplify enrollments and prevent disruption to cash flow
- Enrollment Accelerator to enhance the speed and accuracy of the enrollment process by automatically creating provider records and pre-enrollment request
- Auto Eligibility to identify and verify insurance coverage
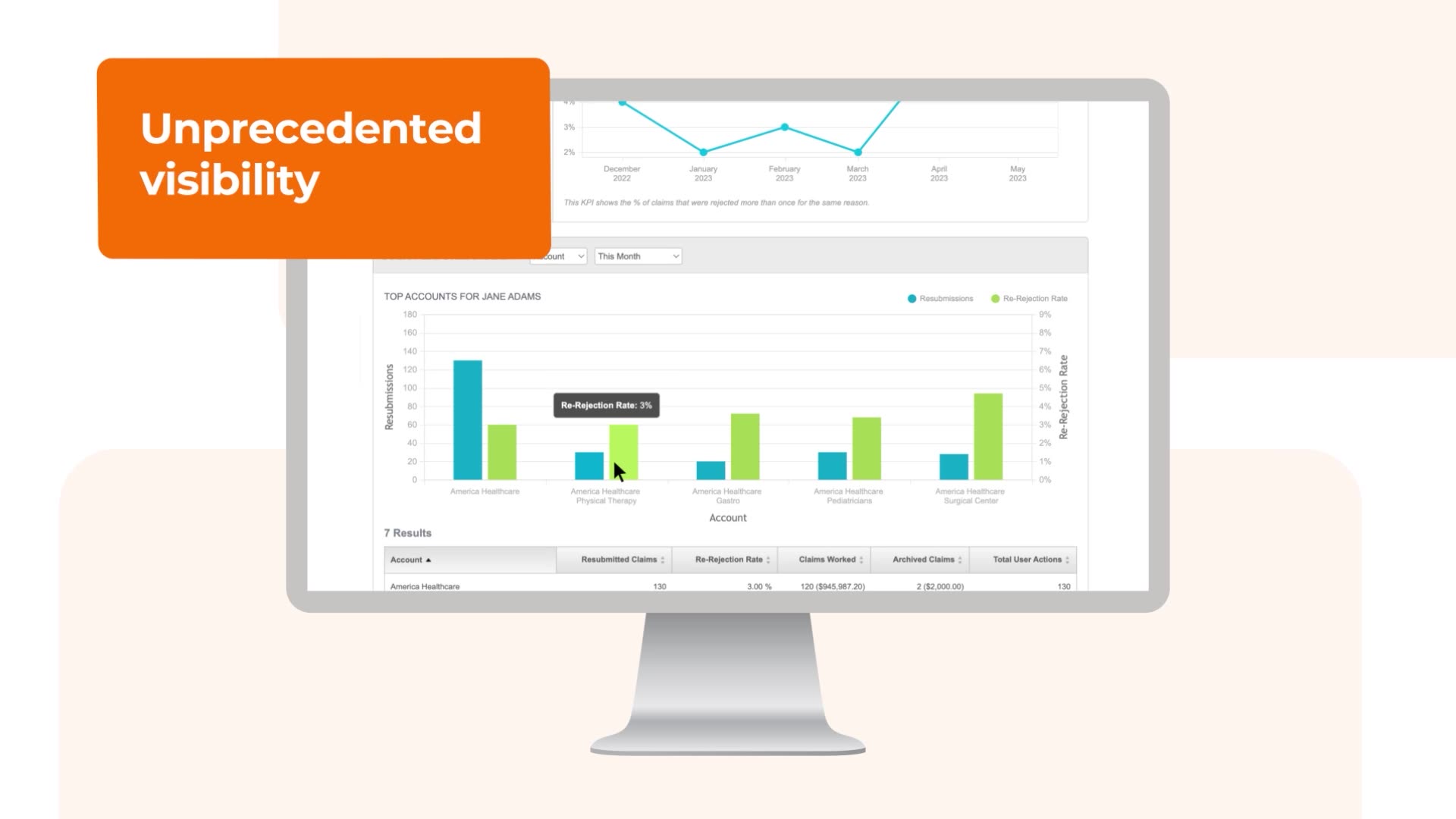
- Dashboards and root-cause reporting to give you transparency and unlock insights
- Coding tools for CPT, ICD, and Revenue Code that make research and validation easy, so you respond accurately to changing coding standards