Leading healthcare organizations like Piedmont, a 26-hospital health system serving 85% of Georgia’s population, are helping shape the future of AI-driven revenue cycle software — while solving real-world challenges today.
Shaping software development + harnessing a unified platform
Piedmont has implemented every product suite from Financial Clearance, Patient Financial Care and Revenue Capture to Claim + Payer Payment Management, Denial Prevention + Recovery, and Analytics + Reporting — so they harness a true end-to-end platform for a completely unified revenue cycle.
“Having an end-to-end solution that integrates well — that just makes a huge difference,” says Sheila Granda, Executive Director of Financial and Operational Effectiveness at Piedmont Healthcare.
As part of Waystar’s Early Adopter Program, Piedmont is was able to be one of the first to leverage innovations in Waystar’s AI-driven Authorization Manager to speed up processing and improve accuracy.
“We’ve been able to influence what’s being built to help support a lot of the issues that we have. Leveraging Waystar, our accuracy rate is in the 90% range, which is tremendous,” says Granda. “We’ve been automating and leveraging more and more AI to get that auth done without any human touch.”
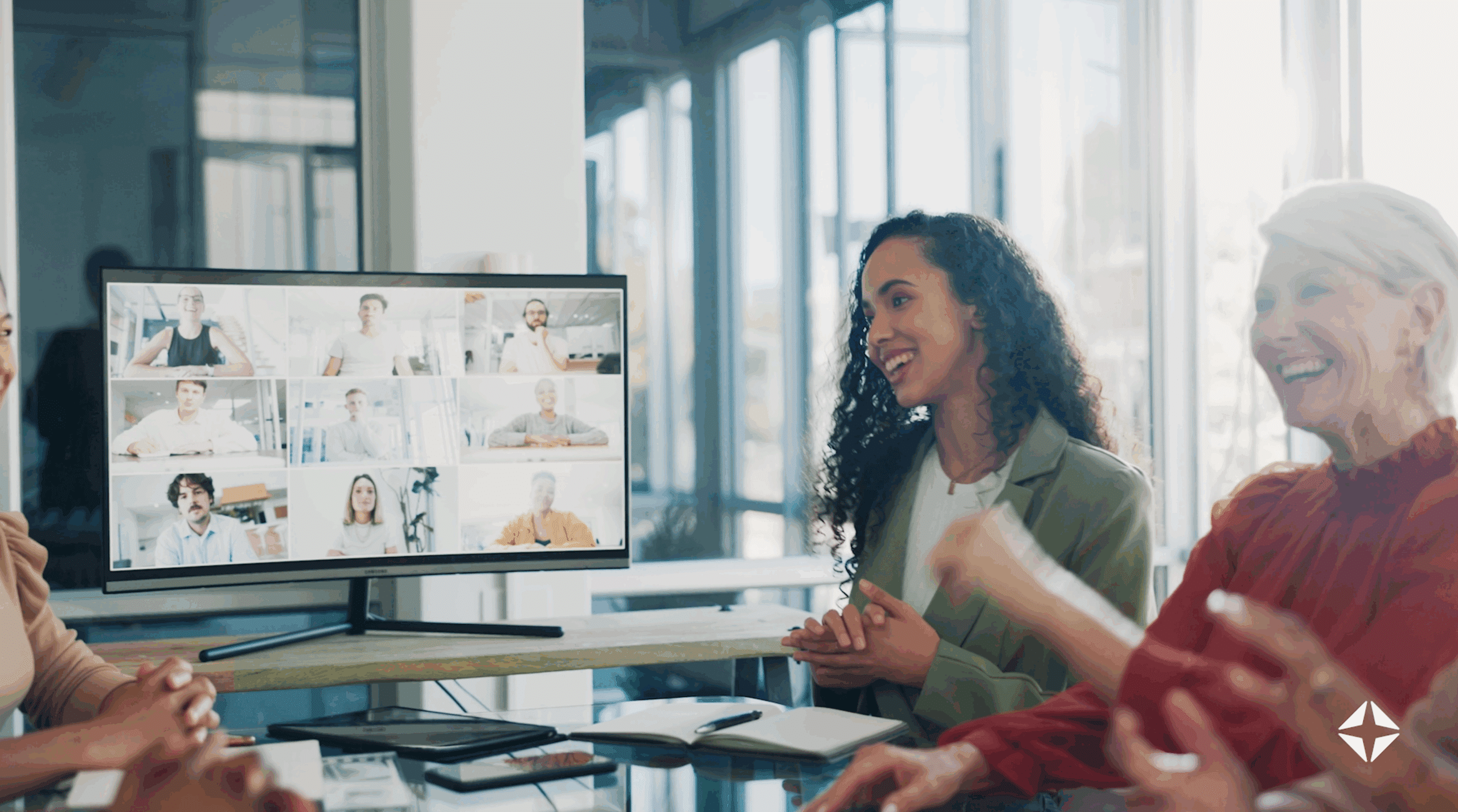
WATCH: Piedmont’s full story
For Piedmont, another differentiator is the partnership with Waystar — one that’s built on collaboration, responsiveness, and trust.
“It is a constant partnership working together. We’ve really valued the knowledge, skills, and really just the friendship and partnership with all of the team,” says Granda.
Piedmont is proving that when a health system and its software partner innovate together, scalable impact is not only possible — it’s already happening.
Learn how you can simplify healthcare payments with Waystar.