As healthcare organizations prepare for shifts in policy and the fast-paced evolution of technology and AI, the Waystar Advisory Board recently convened during our Waystar True North™ Client Conference to share insights on pressing topics: navigating the One Big Beautiful Bill Act (OBBBA), accelerated adoption of AI in revenue cycle management (RCM), payer engagement, and more.
These discussions revealed critical strategies for navigating the future healthcare financial landscape, improving operational efficiency, and preparing for evolving revenue cycle and reimbursement dynamics.
OBBBA: Navigating regulatory change + financial implications
The One Big Beautiful Bill Act (OBBBA) is expected to introduce significant changes to healthcare coverage and reimbursement over the coming years. While the full scope of its impact is still unfolding, members of the Waystar Advisory Board are actively planning and forecast modeling for 2026 and beyond.
To navigate the road ahead while mitigating potential risk and margin impacts, key areas of focus for healthcare revenue cycle leaders include:
- Coverage transitions, particularly in Medicaid and ACA-related programs
- Changes in patient financial responsibility
- Expected variation in states’ funding and resulting policy execution
TOP OBBA IMPACTED AREAS IN RCM
Implications for coverage, collections + Medicaid
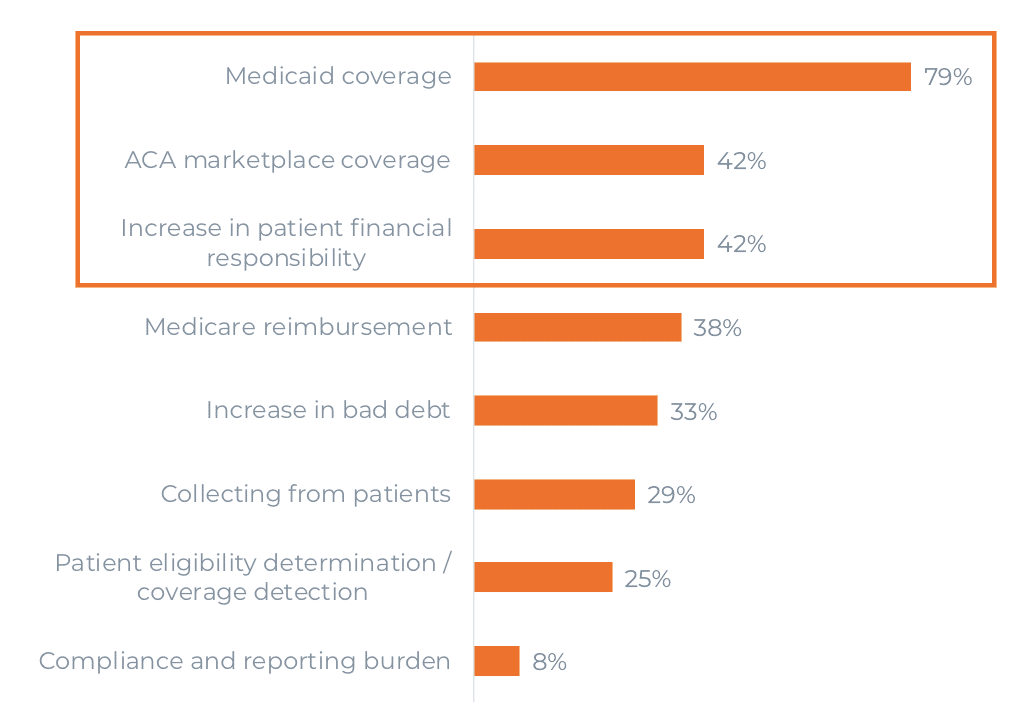
To move from reactive risk management to proactive readiness, members are using this period as an opportunity to strengthen financial modeling and optimize payment strategies.
Learn more about navigating the OBBBA — including implications for the healthcare revenue cycle and actions leaders should take now.
AI in RCM: From pilots to scaled performance
Another key topic covered by the Waystar Advisory Board is AI in revenue cycle management emerging as a powerful lever to improve efficiency and accuracy.
According to a commissioned study conducted by Forrester Consulting on behalf of Waystar, 82% of healthcare leaders now consider AI integral to their RCM operations, with 60% planning to increase investment. Recent survey results from members reflect the same focus on AI in revenue cycle management.
AI ROLE IN RCM STRATEGY
Most members see AI as essential or significant to near-term RCM strategy
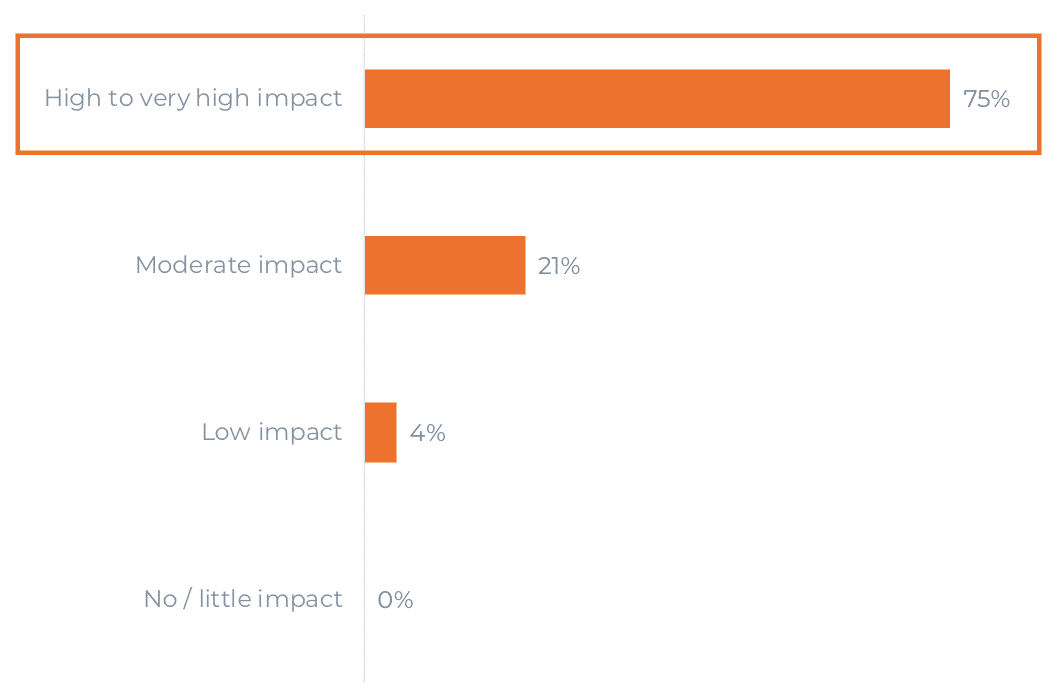
Waystar Advisory Board members also highlighted the need for AI to address key resource-intensive workflows and cited several high-impact areas for AI deployment, including:
- Denial management
- Prior authorization
- Patient communications
Additional focus areas include payment posting, coding, and call center automation.
When it comes to AI in revenue cycle management, the discussions also emphasize the need for human safeguards and integrated platforms to avoid fragmented point solutions and ensure staff adoption.
Discover Waystar’s latest AI-powered software innovations in our recent Waystar Innovation Showcase.
Payer AI usage: Navigating a shifting landscape
As providers begin implementing AI across revenue cycle operations, Waystar Advisory Board members also noted the prevalence of payer AI usage. In fact, 94% of providers expressed concern about payers’ use of AI, especially in the areas of denials, prior authorizations, and audits. Some organizations have started observing increased audits and more complex prior authorization processes, which are already causing reimbursement shifts.
Additionally, nearly half of survey respondents expect resistance to provider AI usage in the next 1-2 years, with many raising concern about how this might influence the dynamic between providers and payers.
Leaders discussed the need for balancing automation to protect revenue while maintaining transparency and fairness in payer relationships. The group saw these dynamics as an opportunity to strengthen scale and prepare for the evolving payer–provider AI balance.
By proactively engaging with payers and leveraging AI to improve accuracy and reduce administrative burden, providers can help create a more balanced and productive payer–provider relationship.
Shaping the future of healthcare payments
The convergence of regulatory changes and technological acceleration presents an opportunity for healthcare leaders. By embracing the shifting financial landscape, advocating for responsible AI adoption, and proactively engaging with payers, healthcare leaders can overcome industry challenges and emerge stronger and more agile.
Join our Waystar True North™ Client Conference 2026 in San Antonio, TX, from August 25-27, 2026, to hear more strategic discussions and innovations transforming the future of the healthcare revenue cycle.