This time of year, rev cycle leaders find themselves asking one question: What changes can providers make now to add real value in the future?
Naturally, the question came up at Reuters Total Health 2022. With economic uncertainty looming, savvy organizations are considering which rev cycle technologies will move the needle. And that consideration starts with a key perspective shift.
It’s time to look at the rev cycle from the patient’s point of view.
In healthcare today, patients are shouldering far more of the financial burden than ever before. Looking at annual averages, single deductibles have increased by 68% over the last 10 years. So, if hard times come and patients can’t afford to pay their part, what happens?
Two things:
1. Patients will stop seeking care.
In 2022, 38% of patients put off treatment because of cost concerns. Without better transparency and more payment options, that percentage will grow.
2. Bad debt will rise for providers.
When insured patients do seek care but can’t afford to pay “their part,” bad debt rises. Today 58% of all bad debt is a result of self-pay after insurance.
On top of that, providers are facing complex regulations, staff shortages, and shrinking margins. Those challenges make it tough to stay afloat, let alone take time to revolutionize the rev cycle.
Healthcare organizations need solutions that deliver a demonstrable return on investment — and they need them now.
3 tactics to add value to the rev cycle through technology
1. Find efficiencies through automation
The pros of impactful automation are widely accepted. With purpose-built solutions, organizations can benefit from:
- Spending less time on manual tasks
- Decreased workloads
- Higher employee satisfaction, and
- Enhanced communications, which leads to
- Higher patient satisfaction and collections.
Prior authorization is a prime example. When you apply automation to that process, the results are transformative.
“Waystar has clients, such as UCHealth, who are seeing a 340% increase in prior authorization speed using automation,” says Matt Hawkins, CEO of Waystar. “That success is possible because we automate so many parts of the process — verification, initiation, unscheduled admissions, notices — and we adapt it all to shifting payer rules and requirements. That creates speed, which does more than just improve productivity — it actually reduces the likelihood of that claim being denied.”
Using automation for prior authorization, UCHealth has seen a 46% reduction in denials related to authorizations.
2. Give your staff the solutions they need
One major goal of technology in RCM is to reduce friction — something that’s crucial in a world where staff shortages are already common. The good news is that every improvement to your healthcare rev cycle makes a difference to the people who use it, and it doesn’t take long for those improvements to take effect.
“The way healthcare infrastructure was built, it doesn’t allow for easy information-sharing prior to care,” says Missy Miller, SVP of Marketing at Waystar. “In every other part of our lives, we expect technology to provide transparency, speed, and accuracy. We order food, we get packages delivered to our door, and we have everything at our fingertips. Patients expect healthcare to deliver the same kind of experience, but holistically, it hasn’t caught up — yet.”
Rev cycle technology can bridge that divide. When you automate tasks and give staff a single, smart platform, change becomes easy.
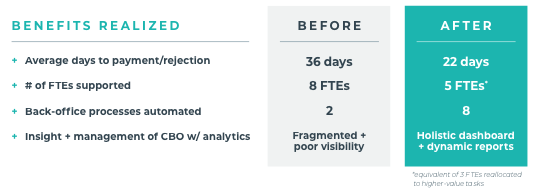
“Take Mount Sinai Health System,” says Miller. “Using an integrated healthcare payments platform, they were able to take advantage of automatic data capture and submission, claims processing and batch management, automated work queues, and much more. By having the right solutions, they saw a 300% increase in back-end automation. When you can remove errors from a process while freeing up employees to work on high-quality initiatives, you can boost collections and satisfaction all at once.”
Read the Mount Sinai Case Study
3. Embrace patient consumerism
In order to make educated decisions, patients want choice, transparency, and accuracy. Providers need technology to meet these demands, and to communicate this information in a personalized way to the patient.
“In the next few years, it’s going to be crucial to unlock true consumerism in healthcare,” says Hawkins. “At Waystar, clients are already using our technology to present highly accurate estimates to patients prior to care. By automating the delivery of accurate estimates, providers are creating payment plans that patients can actually stick to. And we’re seeing dramatic uplift in how those patients are engaging in — and paying for — their healthcare.”
Numbers tell the story for Piedmont Health. Using Waystar’s consumer-centric Patient Payments solution, they’ve seen a:
- 30% increase in point-of-service collections
- 92% collection rate
- $7M payment lift
Much of that boost comes from the fact that those estimates — which are both automated and integrated — are accurate. And that’s just one part of creating a meaningful consumer experience.
“The U.S. Census Bureau did a study that says the lifetime value of a patient is $1.4 million,” says Hawkins. “And Waystar data suggests that there is a significant increase in payments when patients are on a payment plan. Focusing on activities like this — the ones that truly drive patient engagement — is very meaningful. It is such an exciting time to be able to serve providers and patients alike.”
Find this post helpful?
Unlock the 3 P’s of patient consumerism
Want to know more about Waystar Patient Payments?
Discover a better way forward.