
SIMPLIFY HEALTHCARE PAYMENTS
The Waystar
Innovation Lab™
Explore breakthrough AI and advanced automation designed to simplify workflows, eliminate errors, and accelerate revenue — transforming processes for healthcare revenue cycle teams nationwide.
FALL 2025
Waystar Innovation Showcase
Watch the Waystar Innovation Showcase and hear directly from our revenue cycle experts about the AI-powered capabilities driving real, meaningful results across the healthcare revenue cycle.
INNOVATIONS TO OVERCOME RCM CHALLENGES
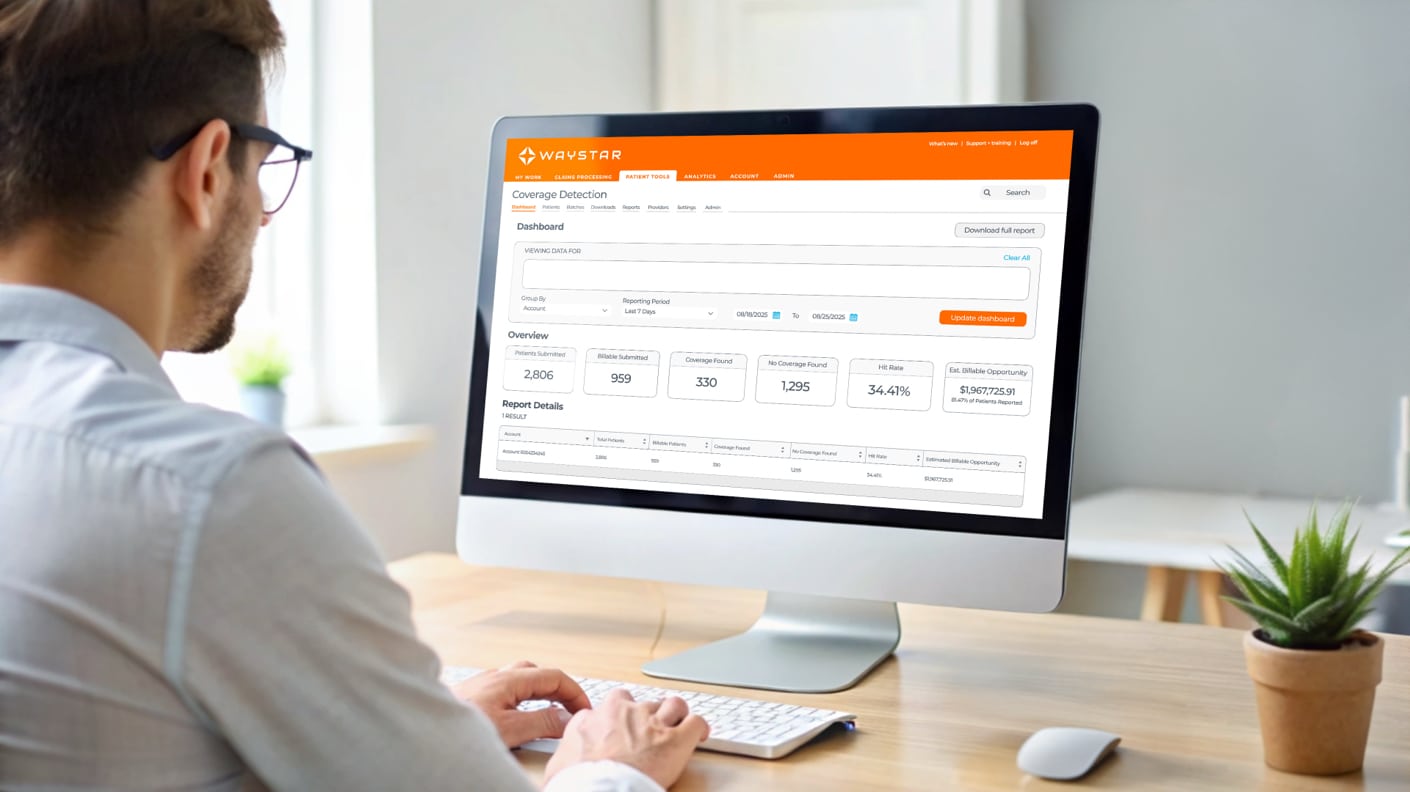
Financial Clearance
Speak to an expert
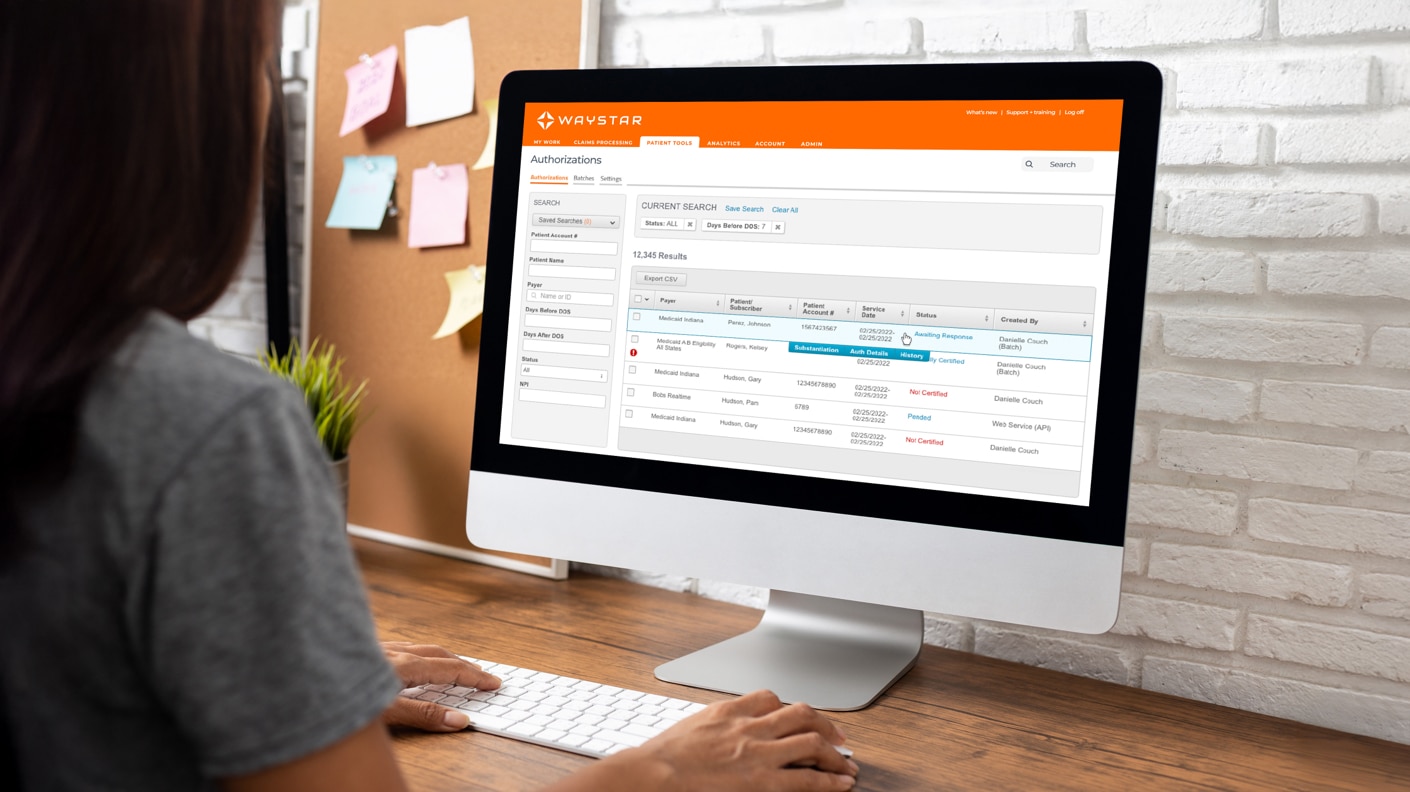
32M
authorization transactions annually
1.2K
payer connections for eligibility
55%
average Coverage Detection hit rate
Waystar data
Patient Financial Care
Get in touch
20-30%
average collections lift
60-80%
average self-service pay rate
61+
patient NPS
Waystar data
Clinical Integrity + Revenue Capture
Request a demo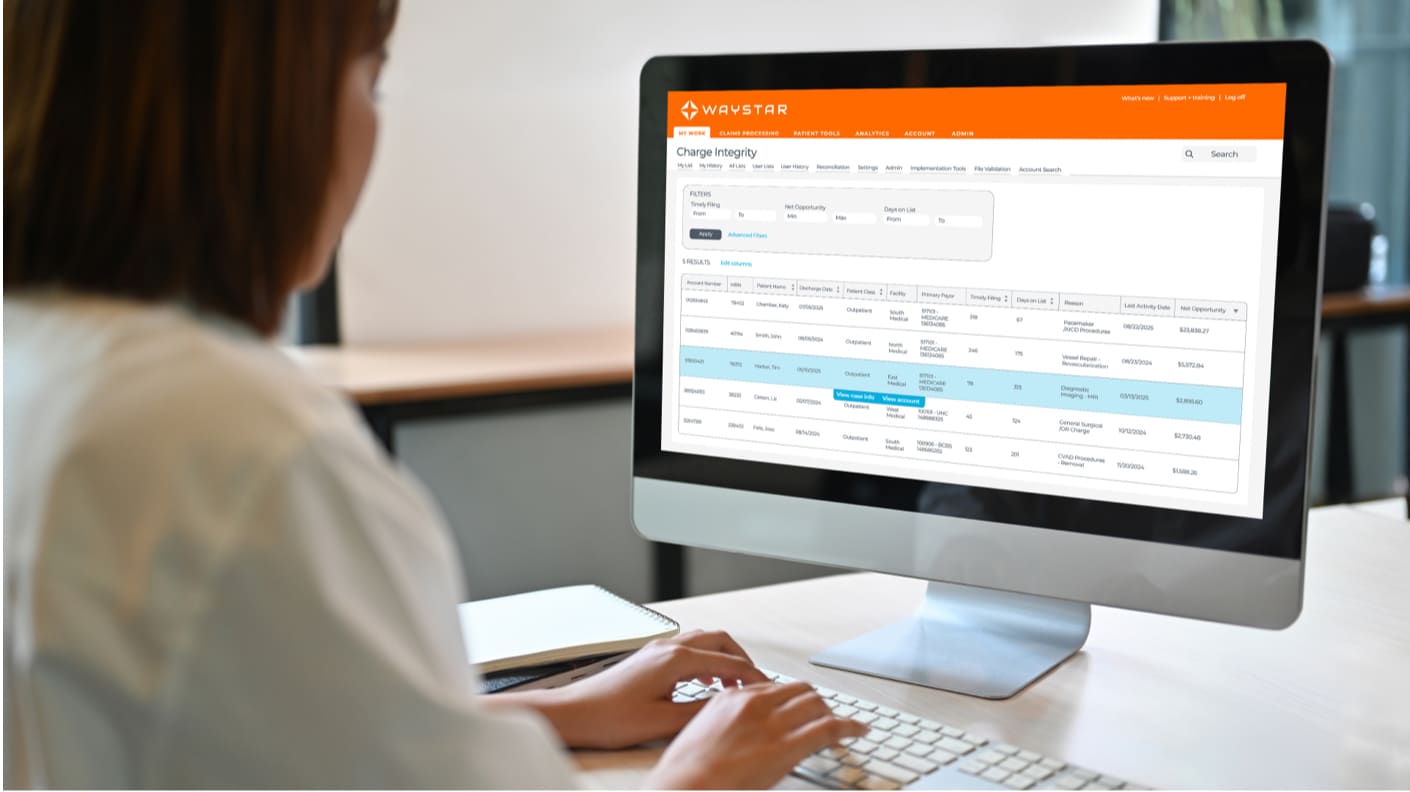
4:1
average ROI for Charge Integrity
$8K
average DRG Anomaly claim recovery
95%
Waystar auditor agreement rates for Charge Integrity + DRG Anomaly
Waystar data
Claim + Payer Payment Management
Connect with an expert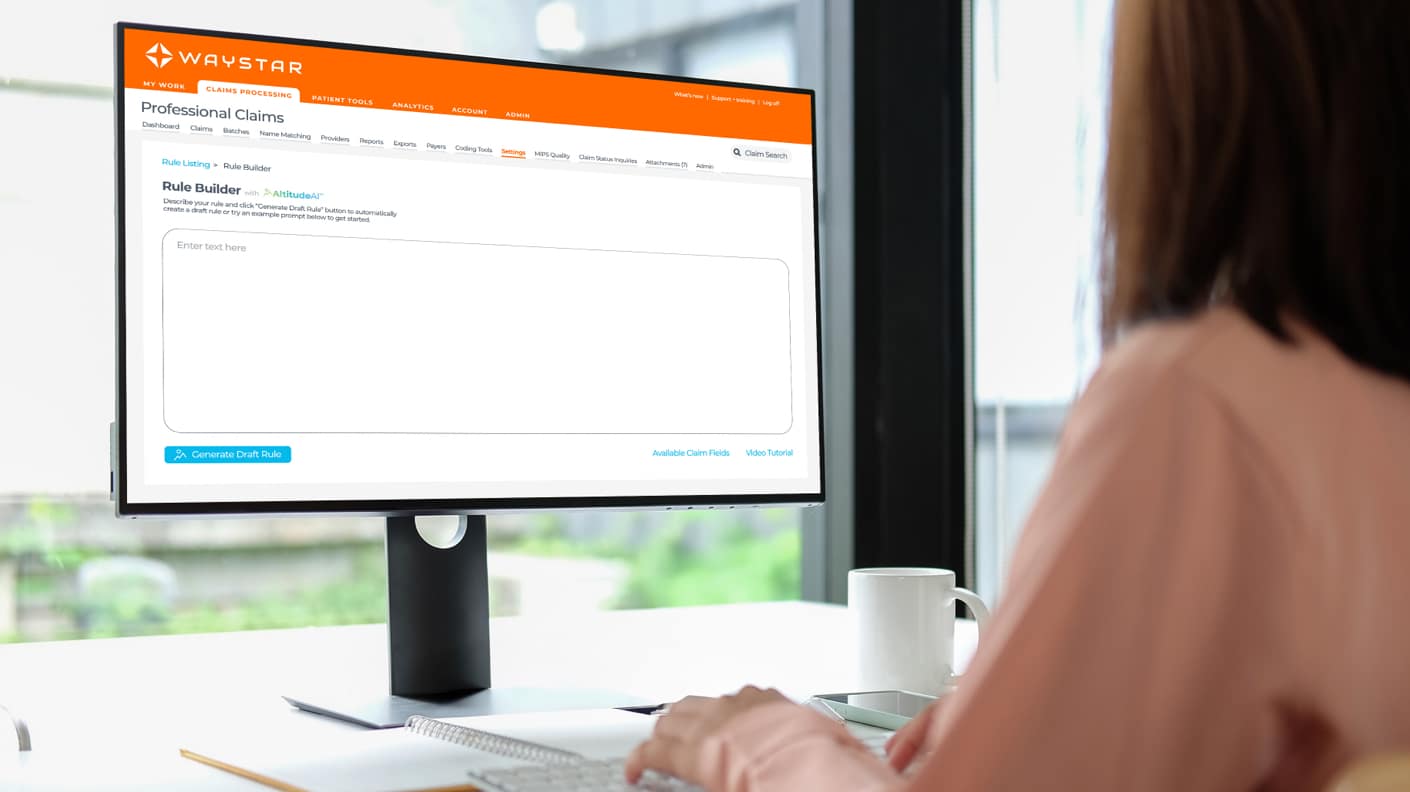
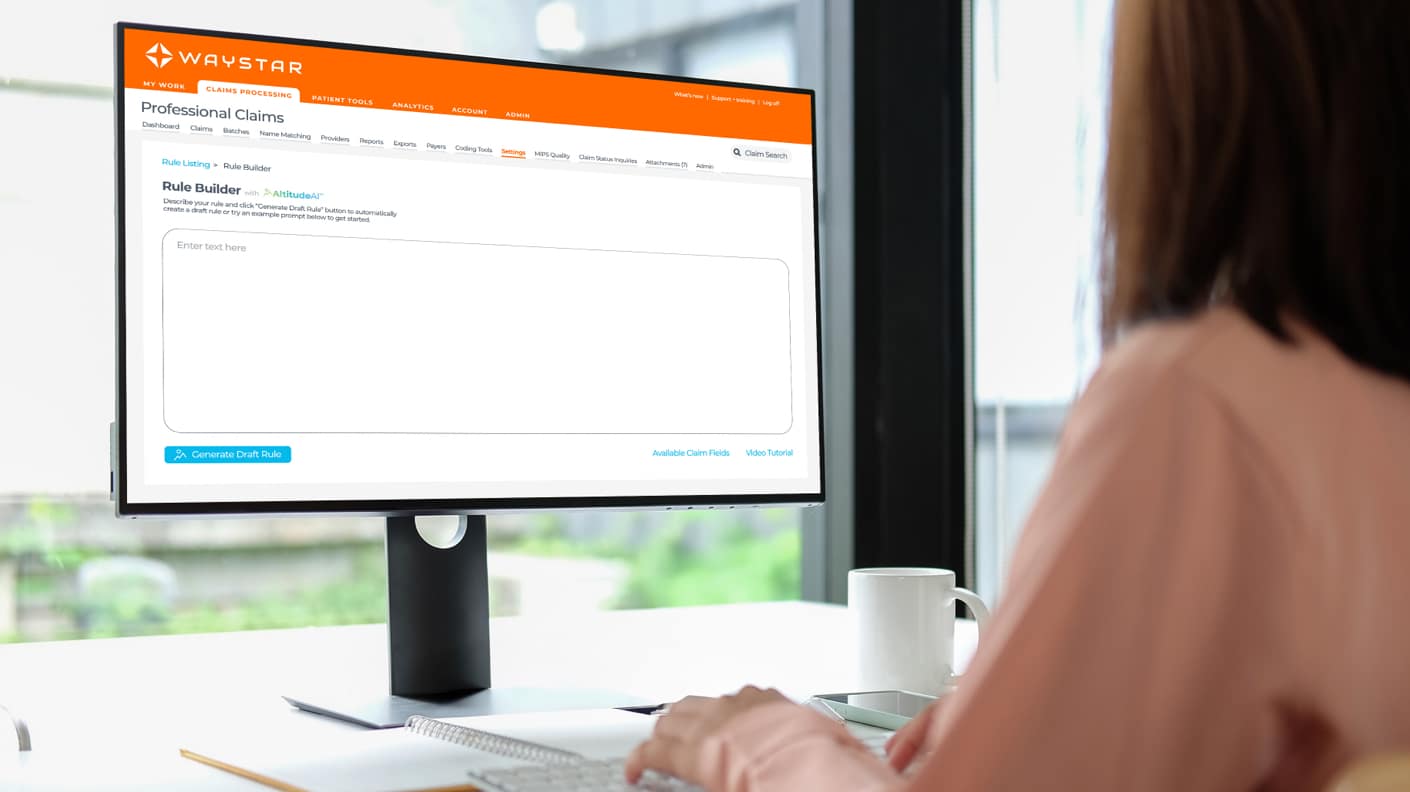
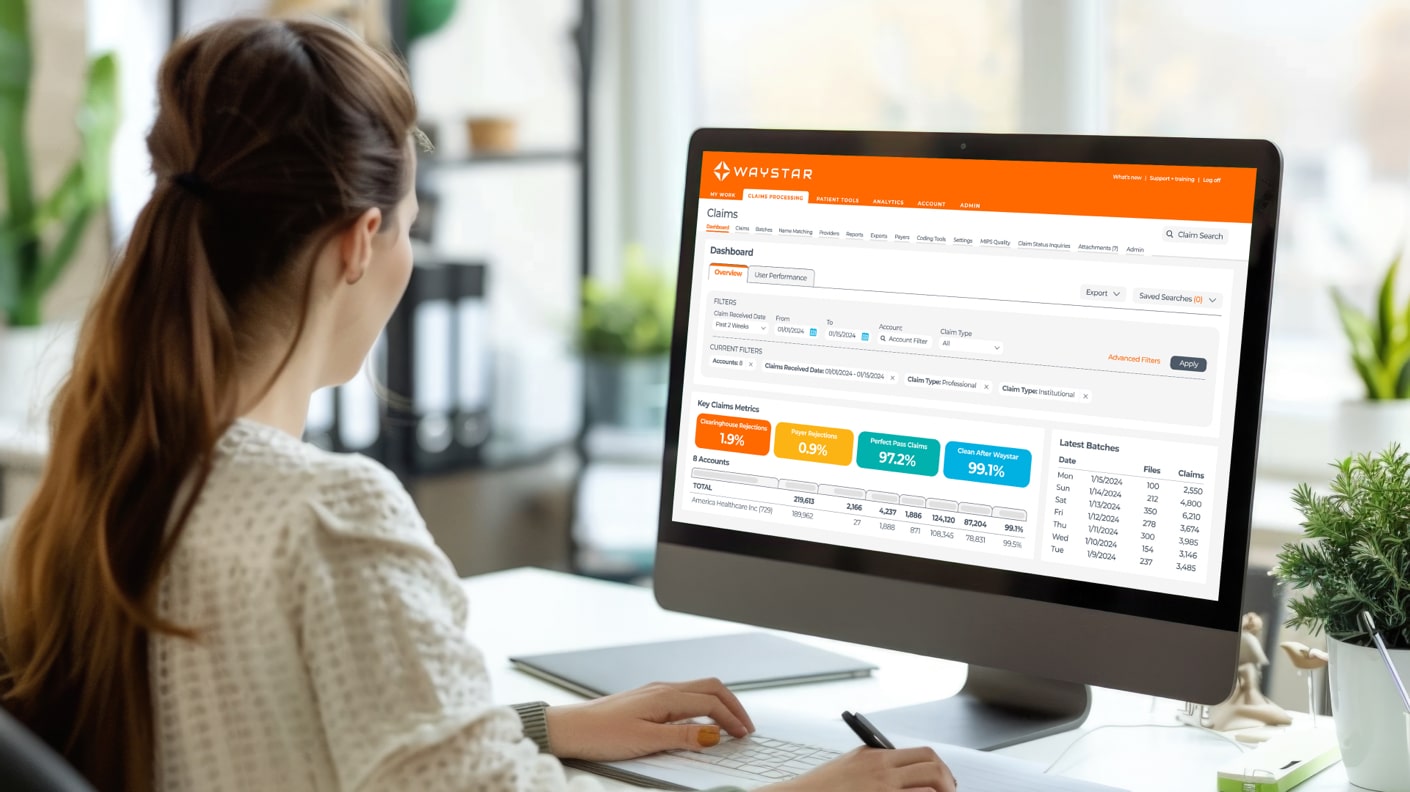
2.5M+
continuously updated edits
5K+
payer connections
98.5%
first-pass clean claim rate
Waystar data
Denial Prevention + Recovery
See it in action3X
Faster appeal package creation with AltitudeAI™
16mins
time savings per appeal package with AltitudeAI™
100%
paperless appeals process
Waystar data
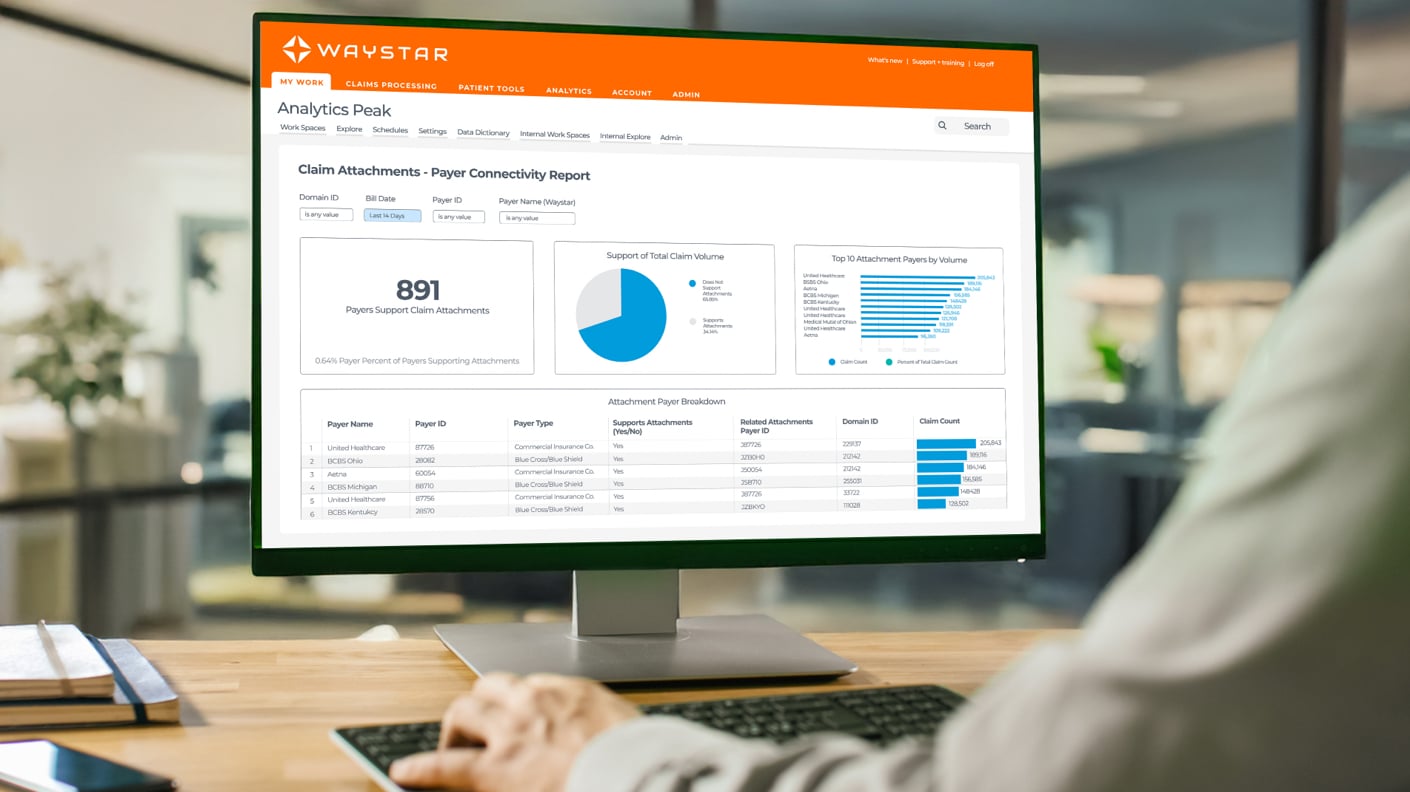
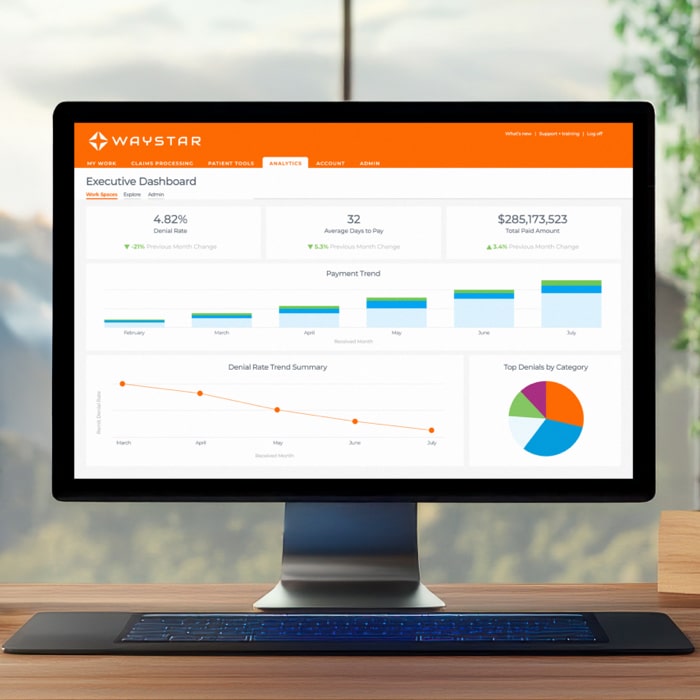
Analytics + Reporting
Book a demo

145+
pre-built KPIs for claims, remits + denials
35+
pre-built revenue cycle specific reports
12
pre-built analytics dashboards for Pro + Peak
Waystar data
LEADING THE WAY IN INNOVATION
innovation1
effectiveness1
ease of use1
1Waystar vs. Competitors, Qualtrics survey (2025)
INNOVATION IN ACTION
Trending resources
Is the status quo costing you?
Speak to a Waystar expert
Curious to learn more about Waystar’s newest innovations? Reach out to speak with a Waystar expert to learn how these solutions can help your healthcare organization see powerful results.








