
Healthcare Denial Management Software
Recover more revenue with Denial + Appeal Manager
When reducing denials is the #1 priority for providers, healthcare denial management software is vital. Otherwise, managing denials and building appeal packages slows cash flow and takes your team off high-value tasks.
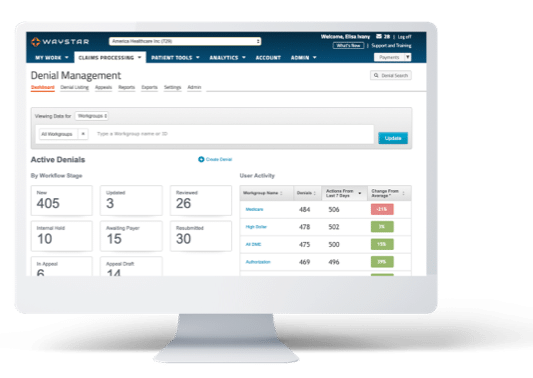
Waystar’s Denial + Appeal Management fixes that. Our software uses AI to track and triage denials — and may even prevent them in the first place. Coupled with paperless, prepopulated appeals forms, our denial management software helps maximize reimbursement and efficiency.
Denial + Appeal Management by the numbers
balance write-off

Proven healthcare denial management software
Speed + maximize reimbursement
Denial + Appeal Management uses Waystar’s massive data sets to prioritize denials likely to result in payment and route them to the right work groups. It leverages a library of 1K+ prepopulated payer-specific forms to generate and submit appeal packages. And it does all this while integrating directly into your PM or HIS. That’s why Waystar clients see results like a 72% decrease in denials rate.
Denial + Appeal Management offers:
- A 100% paperless process + batch appeal submission options to increase efficiency
- AI + predictive analytics to prioritize the denials most likely to be overturned and paid
- Appeal tracking + proof of delivery to eliminate uncertainty
- Customized, exception-based workflows to meet your unique needs
- Advanced analytics + root-cause reporting to support decision-making and denial prevention

Despite being a leader in home health care, BAYADA struggled with an antiquated revenue cycle management system.
With Waystar’s denial management software, they saw:

Transform your revenue cycle with Waystar
Use our smart platform to get even more out of healthcare denial management software — all through a single, cloud-based experience.
Complementary Solutions
Patient Statements | Lockbox | Patient Payments + Portal | Advanced Propensity to Pay | Patient Estimation | Coverage Detection | Charity Screening

Connect with a denial management software expert
Looking for more information on how Denial + Appeal Management can transform your workflows? Fill out the form below, and we’ll be in touch shortly.