AI is one of the most talked-about topics in healthcare payments.
But for leaders, one big question remains: How can my team leverage AI in healthcare revenue cycle management (RCM) today to reduce denials, streamline workflows, and deliver ROI?
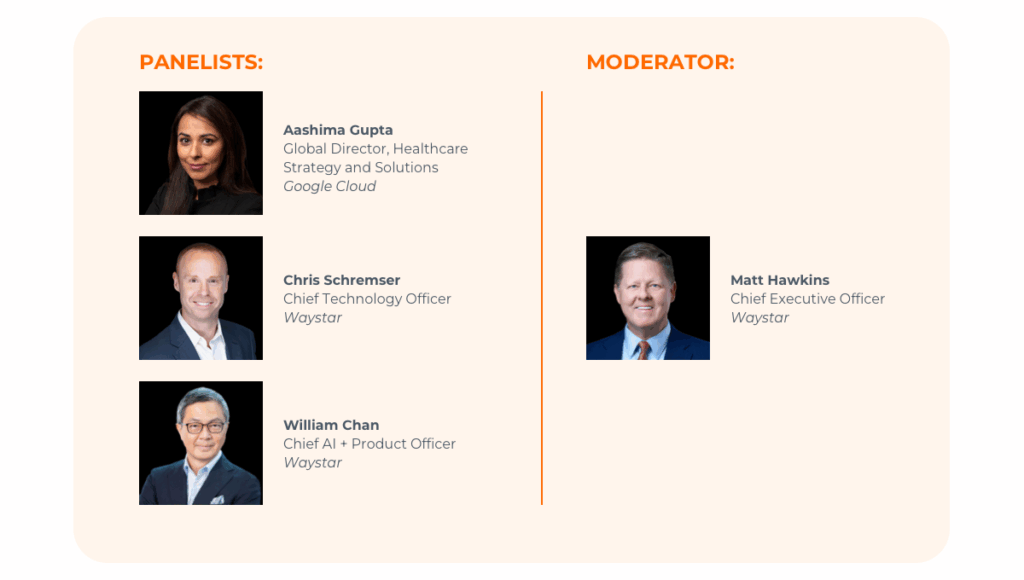
In a recent panel discussion featuring leaders from Waystar and Google Cloud, experts explored what’s delivering ROI now, what to expect next, and why now is the moment to act. Watch the trailer above or view the full discussion here.
4 reasons all AI is not created equal in healthcare revenue cycle management
Healthcare RCM is exceedingly complex. Data is fragmented across systems, workflows are siloed, and regulations add layers of complexity. AI can fix a lot of that — or, rather, good AI can.
“Good AI requires good data, and a good data platform,” says Aashima Gupta, Global Director, Healthcare Strategy and Solutions at Google Cloud. “If you don’t have that, I would not trust the AI.
“Healthcare is a highly regulated, deeply human industry. I cannot overstate the importance of connecting AI to industry-specific data. If AI is not built for the right data, you will create more work, not reduce it.”
Why? Bad, irrelevant, or siloed data causes errors, which wastes time and adds work. And when you’re building AI for healthcare revenue cycle management, siloed data can be particularly insidious.

“Healthcare is so complicated because so many disparate pieces of data must come together,” says William Chan, Chief AI + Product Officer at Waystar. “Revenue cycle is the nexus of clinical, administrative, financial, and payer data, and all four of these use different kinds of data and different workflows. Good AI says, ‘Hey, I need to understand all of this if you want me to help streamline your process.’ That makes interoperability crucial for any AI-driven tool to succeed.”
Finally, leaders reiterated that good AI must keep user data secure.
“The security of our clients’ data remains mission-critical,” says Chris Schremser, Waystar CTO. “Google has built this incredible technology that allows us to keep client data ‘locked up’ so even their engineers can’t access it. Think of it this way: Google creates the lockbox, but we — and our clients — hold the key. As we continue to develop AI for healthcare revenue cycle management, cybersecurity has to come first.”

What’s real today: AI use cases that deliver ROI in healthcare revenue cycle management
Panelists echoed what research shows: Most leaders — 82% — say AI is already an integral part of their organization’s revenue cycle. Here are just three examples the experts discussed.
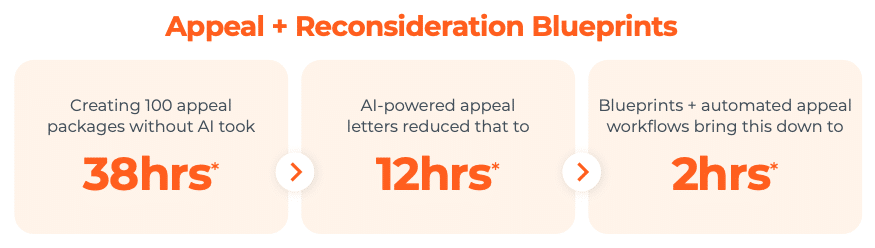
1. AI is generating appeals faster, with less effort
Waystar’s solution generates appeal letters in about one minute instead of 16, reducing the time it takes to create appeal packages by 90%.
2. AI is helping overturn more denials
Appeals created by Waystar’s AltitudeAI™ are more accurate, leading to more revenue recovered.
“We’re not taking humans out of the review process,” says Schremser. “Instead, we’re automating and accelerating the completion of mundane tasks while improving accuracy. And we’re already seeing double-digit accuracy improvements — our AI-generated appeal letters are resulting in payment more frequently than those that humans create alone. That’s a tactical example of how we use good data and good AI to give you the right tools at the right time to drive meaningful improvement.”
3. AI agents are returning humans to human work
With systems that act like assistants — gathering claim data, assembling appeal packages — staff can focus on reviews, decision-making, and other tasks that benefit from being done by real, live humans.
“I don’t think AI will take away our jobs, but it will force us to learn and do things differently,” says Chan. “What AI will do for healthcare revenue cycle management is return humans to do human work. AI will do the administrative work behind the scenes, and the people who deliver healthcare to patients can continue to do that.”
These use cases prove AI isn’t just hype — it’s already improving speed, accuracy, and financial outcomes.
The next 2–3 years: from assistants to agents
Panelists also outlined where they expect AI to go in the short term.
The evolution of AI in healthcare revenue cycle management | |
| Observe | AI analyzes and surfaces insights |
| Assist | AI suggests recommended actions |
| Act | AI agents initiate actions with human oversight |
“AI agents go one step further than analyzing data and suggesting action,” says Gupta. “Agentic AI analyzes data from multiple sources, applies reason, and then acts.”
That’s a big deal when potentially up to 90% of data in healthcare is unstructured.
“Health is inherently multimodal, so data can live in a PDF or spreadsheet or image, none of which can easily interact,” says Gupta. “What AI will do is create a fuller picture of a patient using all the different data points: lab reports, attachments, payer guidelines, medical necessity requirements, and so on. Now, in the end, we won’t just see an X-ray — we’ll see a whole human.”
Then, because the work is based on the full picture of a patient, agentic AI can create an appeal letter that’s built using reason, making it more likely to be successful. It can even test that reasoning with industry-specific data to refine it further.

The risk of waiting too long to implement AI in healthcare RCM
So, what happens if organizations delay adopting AI in RCM?
Panelists were clear:
- Manual, siloed workflows will persist.
- Staffing shortages and administrative waste will continue to drain revenue.
- Payers, who are already deploying advanced AI, will maintain their advantage over providers.
- Organizations will operate at a disadvantage and eventually have to play catch-up.
- Most of all, patients will continue to pay the price.
“I genuinely believe breakthroughs in healthcare bring hope to humanity,” says Gupta. “When we think about Waystar’s mission, it’s not just about overcoming a denied claim. It’s about understanding that, on the other end of all of this, there is a patient who is waiting. To me, the technological breakthroughs are all in service of shifting the conversation from healthcare to care, and back to healing.”
5 steps to build a successful AI strategy in healthcare revenue cycle management
Several action items emerged for any healthcare organizations evaluating AI:
1. Start with a roadmap
Define a 6- to 12-month AI strategy tied to measurable outcomes.
2. Prioritize security early
With sensitive healthcare data, trust and compliance are non-negotiable.
3. Strengthen data foundations
Upgrade data infrastructure, prioritizing:
- Interoperability
- Accuracy
- Security
4. Embed AI into workflows
Success depends on aligning AI with human processes. Start reengineering workflows ASAP and train teams to adapt.
5. Keep humans in the loop
Oversight improves trust, accuracy, and adoption — and it ensures compassion remains a key part of the equation.
“Like Aashima, I think AI can be used for moral good, and in healthcare, we need that,” says Matt Hawkins, Waystar CEO. “We can bring transparency to reimbursement, which is good for patients and providers. We can bring clarity and efficiency to administrative tasks, which will reduce waste. And we can bring compassion and humanity to patients by helping identify those who are eligible for charity care so they can be treated appropriately.
“We can harness AI for good. We can be your partner, bringing fairness and equity to healthcare so that humans can help take care of humans. And we can do wonderful things along the way.”
Where to go from here
At Waystar, we’ve built a single, end-to-end platform that connects data, streamlines workflows, and embeds AI where it matters most — from denial prevention to patient financial care. With unmatched payer connectivity and deep expertise in RCM, we help healthcare organizations unlock ROI while keeping security and compliance at the forefront.
Ready to explore what AI can do for your organization?