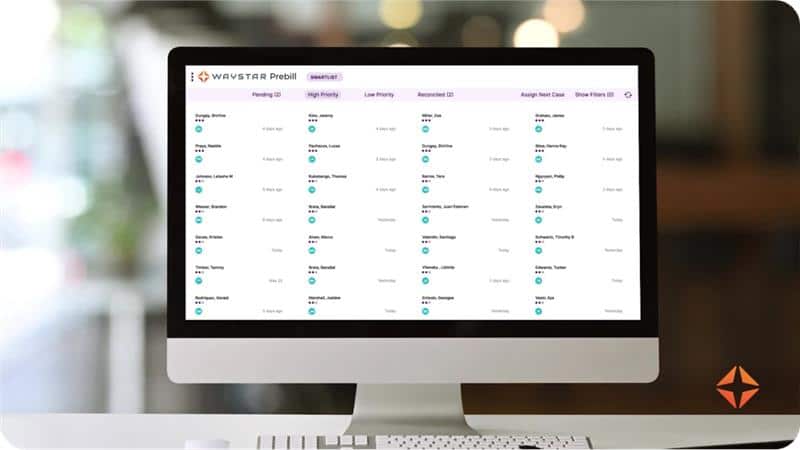
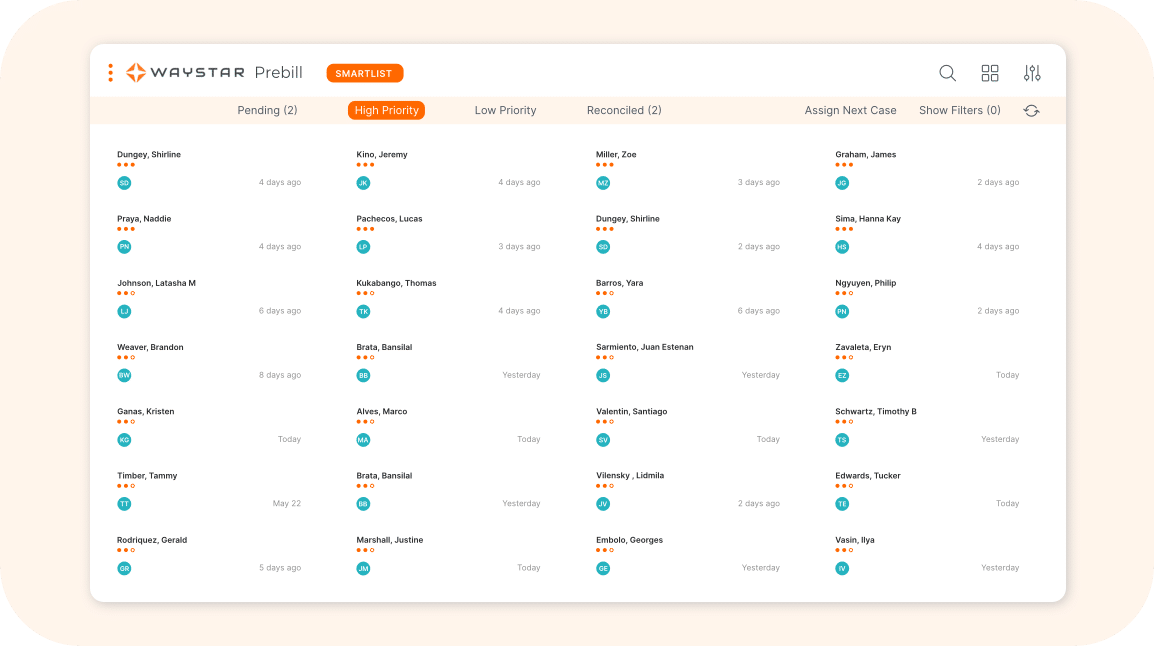
PREBILL ANOMALY DETECTION
Catch documentation gaps. Accelerate payments.
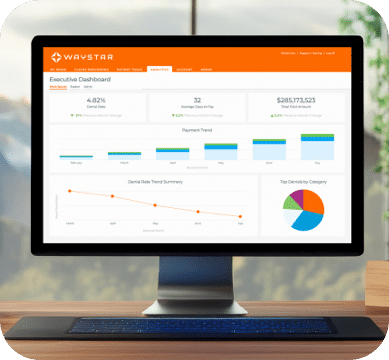
After discharge, 1 in 4 patient encounters still need documentation review¹ — putting critical revenue at risk. Waystar’s AI-powered Prebill Anomaly Detection solution closes those gaps before claims go out, reducing pre-bill revenue leakage and accelerating reimbursement.
¹Waystar, Documentation and Coding Leakage Analysis 2025
Protect revenue + prevent denials
Even with a strong CDI program, critical documentation and coding gaps can still slip through after discharge. Prebill Anomaly Detection pinpoints the reviews that matter most — reducing denials and ensuring fuller, faster reimbursement — without disrupting workflows. See how much you could be capturing with Waystar.
Calculate savings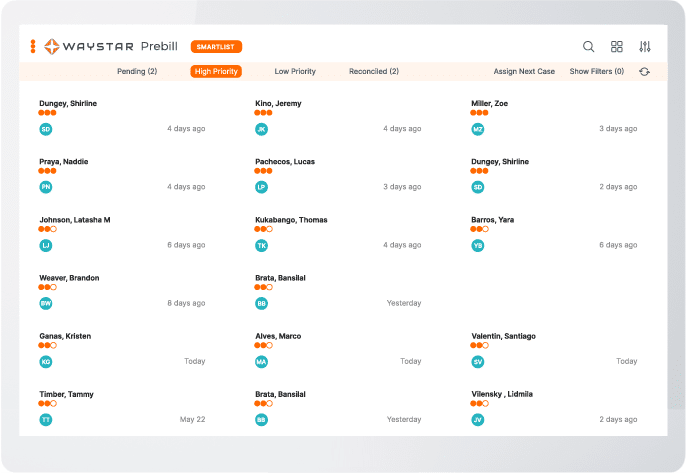
2Waystar, Client Cohort and Model Performance Analysis, 2025
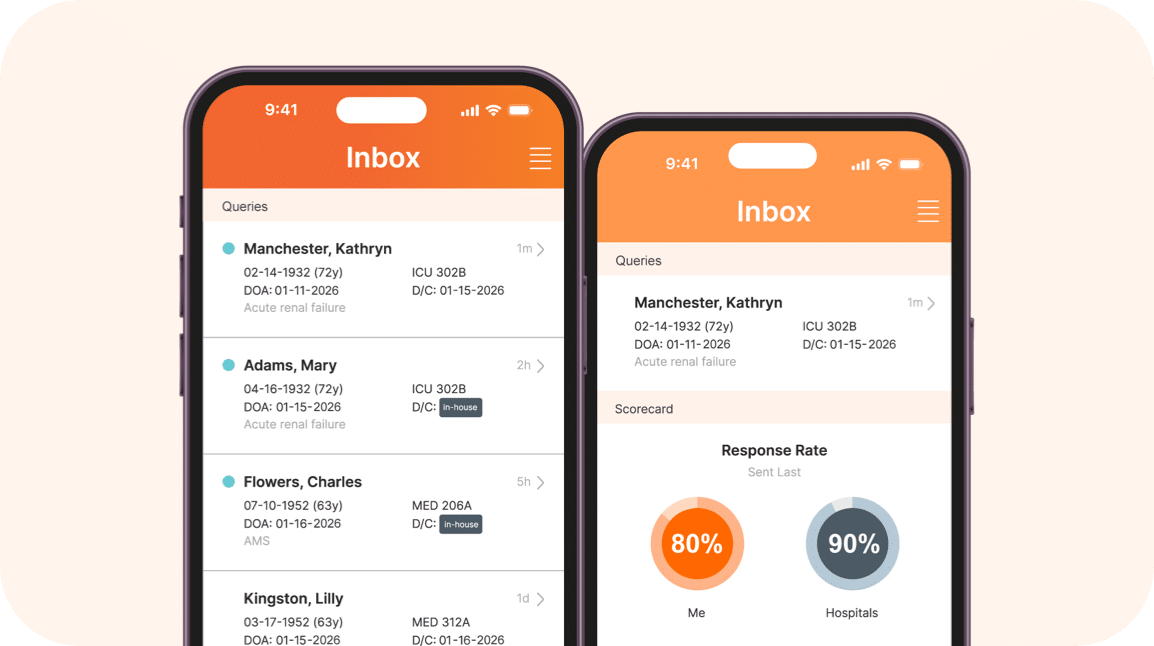
CLINICAL INTELLIGENCE + FINANCIAL INSIGHTS
Smarter documentation.
Stronger payments.
Waystar’s AI-powered Prebill Anomaly Detection works to reduce leakage in the critical stage after discharge and before billing. By targeting inpatient records with meaningful gaps, your team can curb denials and ensure the care delivered is accurately captured.



TRUSTED BY HEALTHCARE LEADERS NATIONWIDE
By The Numbers
$47M
annual net new revenue at a national health system
$14M
annual net new revenue at a south-central health system
$10M
annual net new revenue at a New England health system
97%
physician response rate post-discharge
93%
agreement query agree rate post-discharge
Waystar, Client Cohort and Model Performance Analysis, 2025
Trending resources
Infirmary Health’s way forward
Request a demo of Waystar Prebill Anomaly Detection
See how your healthcare organization can benefit from an AI-powered pre-bill workflow. Reach out to a Waystar expert for a personalized walkthrough today.