BrightSpring’s way forward
Open enrollment continues to intensify eligibility complexity — particularly for Medicare Advantage and Medicaid managed care populations. Coverage changes, patient confusion, and constant plan-switching create downtstream challenges that strain revenue cycle teams.
Tackling open enrollment challenges
For BrightSpring Health Services, a leading provider serving complex populations across more than 1,000 locations, the challenge was clear: move from a reactive approach to eligibility issues to a proactive, automated one.
“A lot of people, especially elderly patients, don’t understand that they signed up for a Medicare Advantage plan. They’re like, ‘What do you mean? My red, white, and blue card isn’t what you need?’” said Linda Rosser, Senior Director of Revenue Cycle at BrightSpring. “But I think that’s kind of a big thing for me: people just don’t really understand what they’re signing up for with their coverage.”
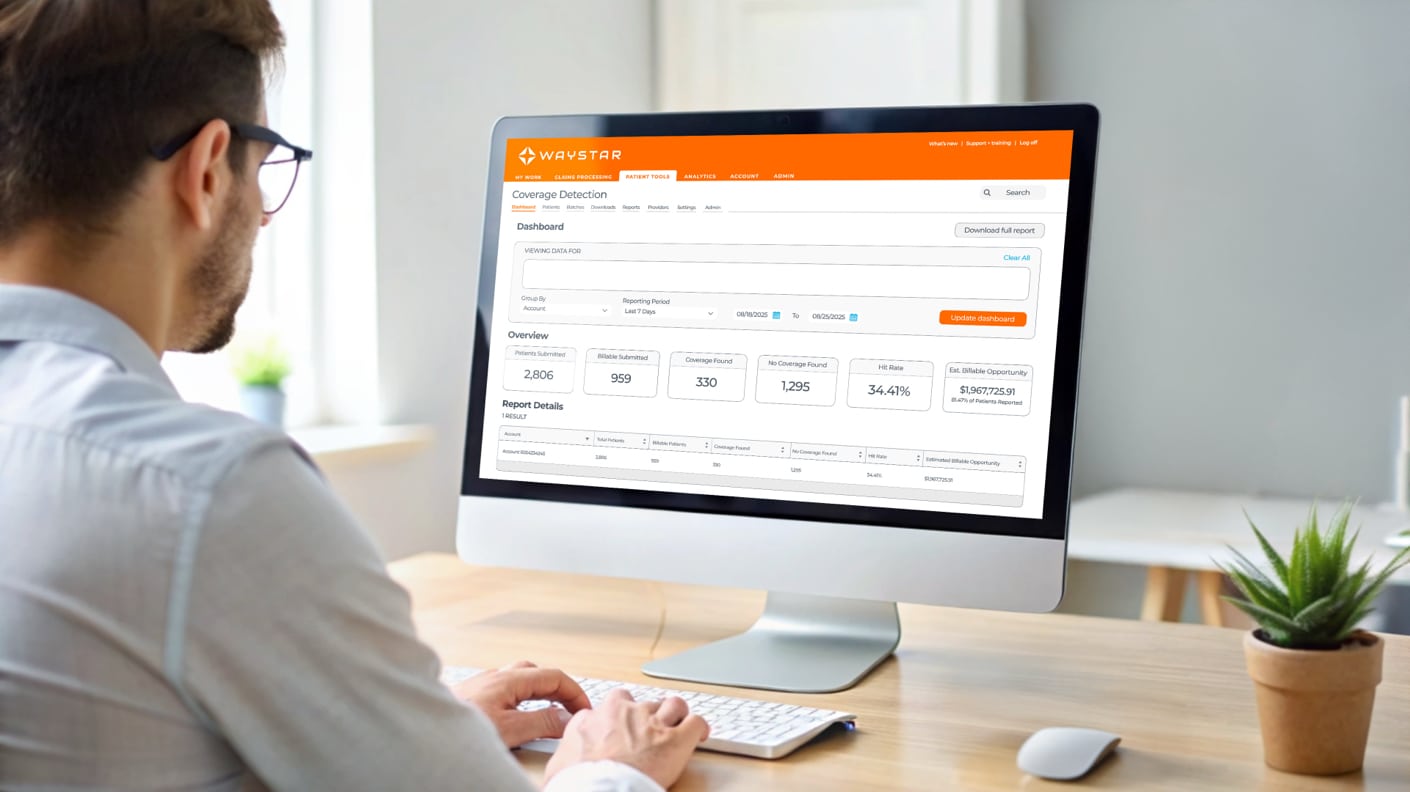
Finding hidden coverage before it becomes a denial
During open enrollment, patients frequently switch Medicaid MCOs or Medicare Advantage plans without notifying providers — leaving teams to discover changes only after claims are rejected or denied. With Waystar, BrightSpring implemented Coverage Detection to ensure eligibility accuracy at multiple points in the workflow.
“We run coverage detection and find out what the client really has,” Rosser said. “What’s in the system isn’t always the truth.”
Shifting culture from busy work to strategy
Automation didn’t just change workflows — it changed how teams worked. By clearly mapping current and future states, BrightSpring helped staff see automation as an enabler, not a threat.
“Now [jobs] can focus on the important tasks that we need to get accomplished,” said Rosser. “Not the busywork that just kind of, you know, makes the time of day go by faster.”
Meaningful results with a trusted partner
With smart automation and proactive coverage detection, BrightSpring improved eligibility accuracy, reduced downstream disruptions, and created space for teams to operate more strategically — especially during the volatility of open enrollment.
“We should be thinking strategically, and automation gives us that ability and the bandwidth to be strategic instead of being busywork, task-driven everyday,” shared Rosser. “And with our Waystar partnership, as a leader of an organization, I can spend time on strategy now because I don’t have to worry about my team doing a million things to get one response. We have it automated.”
Learn how your organization can stay ahead of open enrollment challenges with Waystar.