Healthcare organizations are reshaping financial operations and administrative workflows across the revenue cycle with AI. Revenue cycle and billing teams are more equipped and empowered to work smarter than ever before. The same opportunity exists in post-acute RCM, where staffing shortages, growing payer complexity, and tighter margins require providers to do more with less.
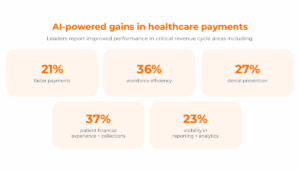
According to a commissioned study conducted by Forrester on behalf of Waystar, healthcare organizations adopting AI-powered software see meaningful results in key focus areas. Leaders report improved performance in critical revenue cycle areas including:
- 21% faster payments
- 23% visibility in reporting + analytics
- 27% denial prevention
- 36% workforce efficiency
- 37% patient financial experience and collections
For skilled nursing facilities, rehabilitation centers, home health agencies, and long-term care providers, the path forward is clear: Leveraging AI and automation streamlines workflows while accelerating cash flow and empowering team members to deliver excellent patient and family financial care.
Read on to learn 5 ways you can harness AI for smart post-acute RCM.
1. Streamlining workflows + boosting workforce efficiency
It’s typical for post-acute care staff to juggle high volumes of billing, authorizations, and payer follow-ups — with limited resources. But surveyed leaders reported that AI improved workforce efficiency by 36%. Can you imagine getting more than a third of your day back to focus on more important things?
AI can relieve pressure from overwhelmed teams by handling repetitive or tedious tasks, identifying priorities, and providing real-time recommendations.
Specifically, today’s RCM software innovations can automatically:
- Verify benefits for new patient admissions
- Flag claim errors before submission
- Predict which denials are most likely to be overturned
- Create time-consuming appeal documentation
With these capabilities, staff can focus on higher-priority work while improving accuracy in post-acute RCM.
See how one healthcare organization uses the latest innovations to eliminate repetitive tasks so teams can focus on higher-value work.
2. Preventing avoidable denials + accelerating appeals in post-acute RCM
Denials continue to erode margins in post-acute settings, particularly as Medicare Advantage and managed Medicaid requirements grow more complex. But with AI, the future for post-acute care organizations looks brighter. Surveyed leaders reported a 27% improvement in denial prevention with AI, a meaningful operational shift that reduces administrative strain and protects revenue for post-acute providers.
Advanced automation is helping prevent frontend denials by keeping upfront processes like eligibility and authorization more accurate in real-time. For denials that do happen, predictive analytics can identify claims with the highest probability of payment, helping teams focus their efforts where they matter most. Generative AI continues to evolve, helping staff manage denials and rejections effectively while autonomously drafting appeal and reconsideration letters.
Ultimately, advancements in generative AI result in:
- Cleaner claims
- Less time working appeals
- A better overturn rate
- Fewer write-offs
Watch how three health organizations prioritize claims, resolve denials, and accelerate the appeal process with automation, predictive analytics, and generative AI.
3. Accelerating cash flow with faster payments
Post-acute organizations often face long payment cycles due to eligibility issues, documentation requirements, and payer delays. But surveyed healthcare organizations using advanced automation and AI-powered claim management are seeing payments arrive 21% faster, directly improving days in A/R and predictability of cash flow — two critical financial health indicators in post-acute RCM.
One way providers can keep cash coming in is by gaining real-time visibility into claim status and proactively resolving bottlenecks — fast. When there is a slowdown with a claim, RCM solutions can provide timely updates about actions to take and recommend rules based on what is happening as claims flow between your system and payers.
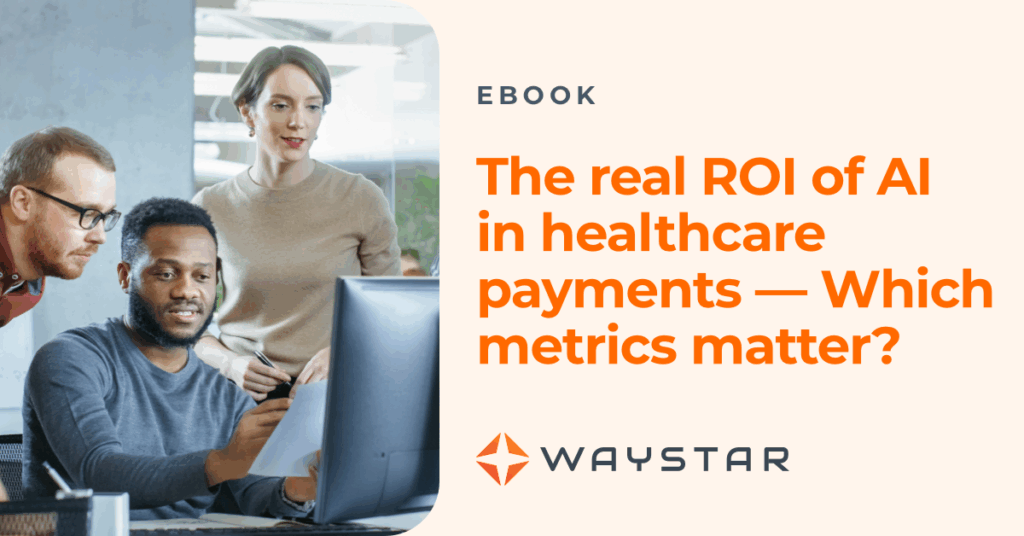
Learn more about which metrics matter most when it comes to integrating AI into your revenue cycle in our eBook, The ROI of AI in healthcare payments: Which metrics matter?
4. Enhancing the family financial experience in post-acute RCM
Families already navigating a complex care journey shouldn’t have to wrestle with confusing bills or unclear balances. The Forrester study found a 37% improvement in financial experience and collections when organizations use advanced automation and AI to improve financial care for patients and caregivers.
With modern software, post-acute providers can offer a smoother, digital-first experience, including:
- More clarity with accurate estimates and statements with easy-to-understand language
- Less phone time for patients chasing information and staff strapped for time — with digital payment plan options, digital communications, and digital payments
- More time to focus on important tasks
Personalized communications, more accuracy, and transparency not only improve the patient and family caregiver experience — they also reflect positively on your organization’s reputation.
See how one organization partnered with Waystar for more accurate claim submission and billing to elevate their patient financial experience.
5. Gaining visibility + control
AI’s impact goes beyond offloading administrative burden and improving patient care. Leaders need insights to drive smarter decisions. AI and advanced automation-enabled analytics bring 23% better visibility into performance, denial trends, payer mix, and staff efficiency — all in one place.
Executives in post-acute care can monitor metrics across locations, identify bottlenecks, and forecast revenue trends, without relying on manual reports or disconnected systems.
Read our eBook to see how your organization can overcome siloed data and use payment analytics to optimize financial performance starting now.
Move from AI potential to proven ROI
When it comes to the healthcare revenue cycle, AI is no longer theoretical. But how do you ensure AI and advanced automation deliver meaningful, repeatable results in post-acute RCM?
The key is choosing software that seamlessly:
- Handles all the claim types you accept (both government and commercial)
- Takes burden off your team
- Improves financial care for patients and families
- Accelerates cash flow
- Offers insights that lead to improvements — from efficiency to the bottom line
Waystar’s automation and AI-powered revenue cycle software platform is designed to integrate with post-acute organization PMs to do all of this and more.
How else can AI help in post-acute RCM?
Download the full AI in healthcare payments software: A strategic imperative report to explore how leading organizations are using AI to overcome workforce challenges, improve margins, and transform financial operations.